The vagus nerve is a vital component of the human body’s intricate nervous system. As one of the longest cranial nerves, it plays a crucial role in maintaining homeostasis and regulating various bodily functions. However, in some individuals, this important nerve can become overactive, resulting in a range of disorders that can significantly impact their quality of life. Understanding the causes of overactive vagus nerve disorders is essential in order to provide effective diagnosis, treatment, and management. By exploring the triggers behind these conditions, healthcare professionals can gain valuable insights into this complex issue.
Understanding the Vagus Nerve
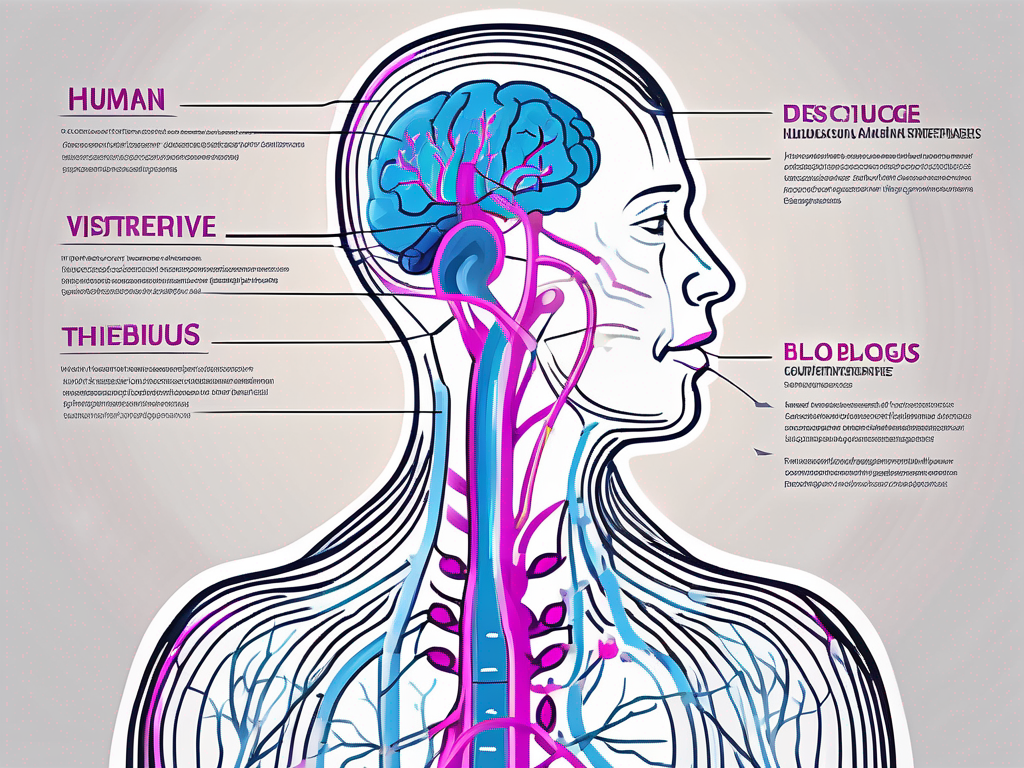
Before delving into the causes of overactive vagus nerve disorders, it is important to have a comprehensive understanding of this significant neural structure. The vagus nerve, also known as the 10th cranial nerve or CN X, originates in the brainstem and extends throughout the body, connecting various organs and tissues to the central nervous system.
The vagus nerve consists of multiple branches that innervate different regions of the body, including the heart, lungs, gastrointestinal tract, and other vital organs. It is responsible for controlling involuntary bodily functions, such as heart rate, digestion, and respiration. Additionally, the vagus nerve plays a crucial role in the parasympathetic nervous system, which is responsible for conserving energy and promoting relaxation.
The vagus nerve’s intricate anatomy allows it to perform its diverse functions. It has both sensory and motor fibers, meaning it can transmit information from the body to the brain and vice versa. This bidirectional communication enables the vagus nerve to regulate various bodily processes and maintain homeostasis.
Anatomy and Function of the Vagus Nerve
The vagus nerve branches out extensively, forming a complex network throughout the body. One of its major branches, the recurrent laryngeal nerve, innervates the muscles responsible for vocal cord movement, allowing us to speak and produce sound. Another branch, the auricular branch, supplies sensory fibers to the external ear, contributing to our sense of hearing.
In addition to its role in controlling vital organs, the vagus nerve also influences the release of neurotransmitters in the brain. It has been implicated in regulating mood, memory, and even social behavior. Studies have shown that stimulating the vagus nerve can have therapeutic effects on conditions such as depression and epilepsy.
The Role of the Vagus Nerve in the Body
Furthermore, the vagus nerve is involved in regulating the body’s stress response, immune system functioning, and even emotional states. It acts as a communication pathway between the brain and other parts of the body, transmitting signals that influence physiological processes and maintaining balance.
When the body is under stress, the vagus nerve helps activate the “rest and digest” response, which counteracts the “fight or flight” response triggered by the sympathetic nervous system. This activation leads to a decrease in heart rate, blood pressure, and respiration, allowing the body to conserve energy and promote healing.
Moreover, the vagus nerve plays a crucial role in the gut-brain axis, a bidirectional communication system between the gastrointestinal tract and the brain. It helps regulate digestion by controlling the release of digestive enzymes and promoting the movement of food through the intestines. This connection between the gut and the brain has been linked to various conditions, including irritable bowel syndrome and anxiety disorders.
In conclusion, the vagus nerve is a complex and multifaceted component of the nervous system. Its extensive network and diverse functions make it a vital player in maintaining overall health and well-being. Understanding the intricate anatomy and functions of the vagus nerve is crucial in comprehending the causes and potential treatments for overactive vagus nerve disorders.
Overactive Vagus Nerve Disorders Explained
Overactive vagus nerve disorders encompass a range of conditions characterized by excessive activity or sensitivity in the vagus nerve. These disorders can manifest in various ways, affecting different body systems and causing distressing symptoms for individuals.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating many bodily functions. It is responsible for controlling heart rate, digestion, sweating, and even certain aspects of mood and cognition. When this nerve becomes overactive, it can lead to a cascade of symptoms that can significantly impact a person’s quality of life.
Symptoms and Diagnosis
The symptoms of overactive vagus nerve disorders can vary widely depending on the specific condition and the affected body systems. Common symptoms may include excessive perspiration, dizziness, gastrointestinal disturbances, abnormal heart rhythms, and even fainting episodes.
Excessive perspiration, also known as hyperhidrosis, can be particularly distressing for individuals with overactive vagus nerve disorders. It can occur in various parts of the body, such as the palms, armpits, or feet, and can be triggered by seemingly mundane activities or situations, such as eating spicy food or feeling anxious.
Dizziness is another common symptom that individuals with overactive vagus nerve disorders may experience. It can range from a mild sensation of lightheadedness to severe vertigo, making it difficult to perform daily activities.
Gastrointestinal disturbances are also prevalent in these disorders. They can manifest as nausea, vomiting, abdominal pain, bloating, and altered bowel movements. These symptoms can significantly impact a person’s ability to eat, digest food properly, and maintain a healthy weight.
However, diagnosing these disorders can be challenging as the symptoms often overlap with other medical conditions. Healthcare professionals rely on clinical evaluations, medical history analysis, and specialized tests to confirm the presence of an overactive vagus nerve disorder.
During a clinical evaluation, healthcare professionals may ask detailed questions about the individual’s symptoms, medical history, and lifestyle factors. They may also perform a physical examination to assess the functioning of various body systems.
In some cases, specialized tests may be necessary to pinpoint the exact cause of the overactive vagus nerve disorder. These tests can include electrocardiograms (ECGs) to evaluate heart rhythm abnormalities, tilt table tests to assess vasovagal syncope, and gastrointestinal tests to identify functional gastrointestinal disorders.
Common Types of Vagus Nerve Disorders
Among the various types of overactive vagus nerve disorders, two common conditions stand out: vasovagal syncope and functional gastrointestinal disorders (FGIDs).
Vasovagal syncope is characterized by sudden fainting episodes triggered by certain stimuli, such as emotional stress or standing up too quickly. These episodes occur due to a temporary drop in blood pressure and heart rate, leading to a brief loss of consciousness. While vasovagal syncope is usually harmless, it can be alarming and disruptive to daily life.
On the other hand, FGIDs encompass a group of disorders that affect the digestive system, causing symptoms like abdominal pain, bloating, and altered bowel movements. These disorders include conditions such as irritable bowel syndrome (IBS), functional dyspepsia, and functional constipation. FGIDs can significantly impact a person’s quality of life, leading to discomfort, dietary restrictions, and social limitations.
It is important to note that overactive vagus nerve disorders are complex and multifaceted. Each individual may experience a unique combination of symptoms and require personalized treatment approaches. Managing these disorders often involves a multidisciplinary approach, including medication, lifestyle modifications, and psychological support.
Unveiling the Triggers of Overactive Vagus Nerve
Identifying the triggers behind overactive vagus nerve disorders is crucial for effective treatment and management. While the precise causes are not yet fully understood, several factors have been implicated in the development and exacerbation of these conditions.
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in regulating various bodily functions, including heart rate, digestion, and immune response. When the vagus nerve becomes overactive, it can lead to a range of symptoms, such as rapid heart rate, digestive disturbances, and anxiety.
Genetic Factors
Studies suggest that genetic predisposition may play a role in the development of overactive vagus nerve disorders. Certain genetic variations and mutations may contribute to altered vagus nerve functioning, leading to increased sensitivity or hyperactivity. Further research is necessary to determine the specific genes involved and their mechanisms of action.
Understanding the genetic factors involved in overactive vagus nerve disorders can provide valuable insights into potential treatment targets. By identifying specific genes or genetic pathways, researchers may be able to develop targeted therapies that can effectively modulate vagus nerve activity and alleviate symptoms.
Environmental Triggers
Environmental factors, such as exposure to toxins, chemicals, or certain medications, have been linked to the onset of overactive vagus nerve disorders. Additionally, head injuries and trauma can disrupt the normal functioning of the vagus nerve, potentially leading to an overactive state. Understanding these environmental triggers is crucial in mitigating the risk of developing these disorders.
Exposure to environmental toxins, such as heavy metals or pesticides, can have a profound impact on the vagus nerve. These substances can interfere with the nerve’s signaling pathways, leading to dysregulation and overactivity. By identifying and minimizing exposure to these harmful substances, individuals may be able to reduce their risk of developing overactive vagus nerve disorders.
Lifestyle and Dietary Influences
The vagus nerve can be influenced by various lifestyle and dietary choices. Chronic stress, poor sleep quality, and unhealthy eating habits can all contribute to vagus nerve dysfunction. Similarly, certain foods and beverages, such as caffeine and alcohol, have been associated with increased vagus nerve activity. Adopting a healthy lifestyle and making mindful dietary choices may help manage symptoms and promote vagus nerve balance.
Stress, a common feature of modern life, can have a profound impact on the vagus nerve. Chronic stress can lead to an overactive vagus nerve, perpetuating a cycle of anxiety and physical symptoms. Incorporating stress-reducing techniques, such as meditation, deep breathing exercises, and regular physical activity, can help restore vagus nerve balance and improve overall well-being.
In addition to stress, sleep quality plays a crucial role in vagus nerve health. Poor sleep can disrupt the body’s natural rhythms, including vagus nerve activity. Establishing a consistent sleep routine, creating a comfortable sleep environment, and practicing good sleep hygiene can support optimal vagus nerve functioning.
Furthermore, dietary choices can significantly impact the vagus nerve. Certain foods and beverages, such as processed foods, high-sugar items, and artificial additives, can trigger inflammation and disrupt vagus nerve activity. On the other hand, a diet rich in whole foods, such as fruits, vegetables, and lean proteins, can provide the necessary nutrients for proper vagus nerve function.
By making conscious lifestyle choices, individuals can positively influence their vagus nerve health and potentially reduce the risk of developing overactive vagus nerve disorders. It is important to consult with healthcare professionals for personalized advice and treatment options.
The Impact of Overactive Vagus Nerve Disorders
Overactive vagus nerve disorders can have profound effects on both physical health and mental well-being. Understanding the implications of these conditions is vital in order to provide appropriate care and support for affected individuals.
Physical Health Consequences
Overactive vagus nerve disorders can significantly affect various bodily functions and lead to a range of physical health consequences. These may include increased heart rate variability, gastrointestinal disorders, chronic pain, and disturbances in breathing patterns. Managing these physical health manifestations is crucial to minimize the overall impact on individuals’ well-being.
Mental Health Implications
In addition to the physical ramifications, overactive vagus nerve disorders can also take a toll on mental health. Many individuals experience heightened anxiety, panic attacks, and feelings of distress due to the unpredictable nature of the symptoms. Addressing the mental health implications of these disorders and implementing appropriate support strategies is essential for comprehensive care.
Treatment and Management of Overactive Vagus Nerve Disorders
Developing effective strategies for the treatment and management of overactive vagus nerve disorders is essential to enhance the quality of life for those affected. An integrated approach that combines medical interventions, natural remedies, and lifestyle changes can significantly alleviate symptoms and mitigate the impact of these disorders.
Medical Interventions
Medical interventions for overactive vagus nerve disorders typically involve pharmacological treatments aimed at stabilizing vagus nerve activity. Medications such as beta-blockers, anticholinergic drugs, and selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help regulate heart rate, reduce gastrointestinal symptoms, and manage anxiety. However, it is important to note that the effectiveness of these medications can vary among individuals.
Natural Remedies and Lifestyle Changes
In addition to pharmaceutical options, natural remedies and lifestyle changes can play a significant role in managing overactive vagus nerve disorders. Techniques such as deep breathing exercises, meditation, and yoga have been shown to promote vagus nerve balance and relaxation. Furthermore, adopting a healthy diet, regular exercise routine, and stress management strategies can contribute to overall well-being and symptom reduction.
Future Research Directions in Treatment
The field of overactive vagus nerve disorders is still relatively understudied, leaving many questions unanswered. Future research is necessary to enhance our understanding of the underlying mechanisms and develop more targeted treatment approaches. Investigating the potential of neuromodulation techniques, such as vagus nerve stimulation, holds promise for advancing the therapeutic options available.
In conclusion, understanding the causes of overactive vagus nerve disorders is essential in order to provide appropriate care for those affected. By unraveling the triggers behind these conditions, healthcare professionals can tailor treatment plans and empower individuals to manage their symptoms effectively. With further research and advancements in medical care, there is hope for improved outcomes and enhanced quality of life for those living with overactive vagus nerve disorders.