The vagus nerve, also known as the tenth cranial nerve, plays a fundamental role in regulating various bodily functions and maintaining homeostasis. Understanding the intricate anatomy and crucial functions of the vagus nerve is pivotal in comprehending the impact of disorders associated with this vital nerve. This overview provides a comprehensive examination of the vagus nerve, common disorders affecting its functionality, the impact on daily life, as well as the advances in research pertaining to these disorders.
Understanding the Vagus Nerve
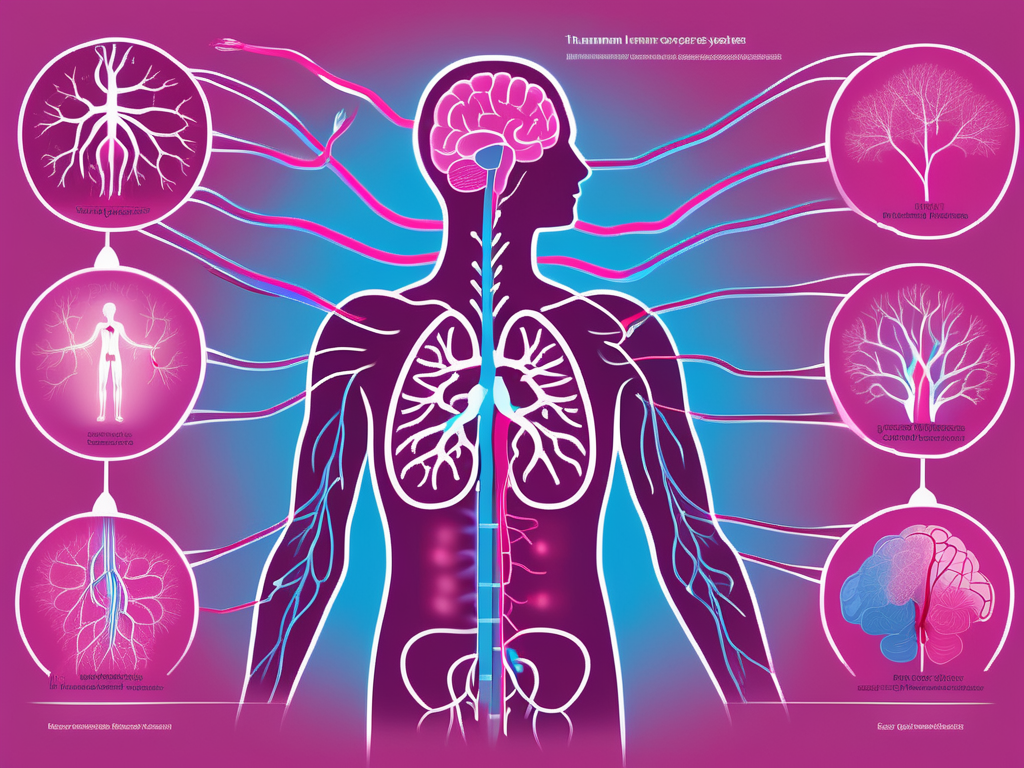
The vagus nerve, originating from the medulla oblongata in the brainstem, is the longest cranial nerve. It extends through the neck, chest, and abdomen, innervating various organs and structures along its path. The word ‘vagus’ means ‘wandering’, aptly describing its complex and extensive network of fibers. The vagus nerve consists of sensory and motor fibers, enabling two-way communication between the brain and multiple organ systems.
As we delve deeper into the intricacies of the vagus nerve, we discover its fascinating anatomy and functions. Let’s explore!
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of both afferent and efferent fibers. The afferent fibers transmit sensory information from various organs, including the heart, lungs, and gastrointestinal tract, to the brain. This sensory information helps regulate bodily functions and maintain internal balance. On the other hand, the efferent fibers carry motor commands from the brain to the organs, influencing processes such as heart rate, digestion, and breathing.
Imagine a vast network of communication lines connecting the brain to vital organs. That’s the vagus nerve at work! It branches outwards from the brainstem, reaching out to every nook and cranny of our body, ensuring seamless coordination and regulation.
Let’s take a closer look at some of the organs and systems that the vagus nerve innervates:
1. Heart
The vagus nerve plays a significant role in regulating heart rate. It acts as a natural pacemaker, helping to maintain a steady rhythm. When we engage in activities that require a higher heart rate, such as exercise, the vagus nerve adjusts its signals accordingly, ensuring our heart beats in sync with our body’s demands.
2. Lungs
Breathing is an automatic process for most of us, but have you ever wondered how it’s controlled? Well, the vagus nerve has a hand in it! It sends signals to the respiratory muscles, coordinating the inhalation and exhalation process. Additionally, it helps regulate the diameter of the airways, ensuring smooth airflow.
3. Digestive System
When we enjoy a delicious meal, it’s the vagus nerve that kicks off the digestive process. It stimulates the release of digestive enzymes and promotes the movement of food through the gastrointestinal tract. The vagus nerve also plays a role in signaling feelings of fullness, helping us regulate our food intake.
4. Liver and Kidneys
The vagus nerve extends its reach to the liver and kidneys, two vital organs involved in detoxification and waste elimination. It helps regulate blood flow to these organs and influences their overall function, ensuring optimal performance.
These are just a few examples of the organs and systems influenced by the vagus nerve. Its impact goes beyond physical functions, extending to our emotional well-being and cognitive processes.
Research has shown that the vagus nerve is involved in regulating emotions, mood, and cognition. It forms a connection between the brain and the gut, often referred to as the “gut-brain axis.” This connection highlights the influence of the vagus nerve on mental health and overall well-being.
As we continue to unravel the mysteries of the vagus nerve, scientists and medical professionals are discovering new ways to harness its potential. Techniques such as vagus nerve stimulation have shown promise in treating various conditions, including epilepsy, depression, and inflammatory disorders.
The vagus nerve truly is a remarkable part of our nervous system, with its extensive reach and multifaceted functions. Understanding its role and significance opens up new avenues for exploring the intricate connections between our brain and body.
Common Disorders of the Vagus Nerve
Disorders involving the vagus nerve can disrupt its vital functions, leading to a range of symptoms and complications. The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex cranial nerve in the body. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and mood. When the vagus nerve is affected by a disorder, it can have a significant impact on a person’s overall well-being.
Identifying and diagnosing these disorders is essential for appropriate treatment and management. Understanding the various symptoms associated with vagus nerve disorders is crucial in recognizing their impact on daily life. Let’s explore some of the common symptoms and diagnostic methods used in the evaluation of vagus nerve disorders.
Symptoms and Diagnosis of Vagus Nerve Disorders
Vagus nerve disorders can manifest in a variety of ways, depending on the affected area and the specific disruption. Common symptoms may include heart rhythm abnormalities, difficulty swallowing, gastrointestinal issues, dizziness, and even mental health disturbances. These symptoms can vary in intensity and duration, making it challenging to pinpoint the exact cause without a comprehensive evaluation.
It is essential to consult a healthcare professional for accurate diagnosis, as symptoms can often be nonspecific and overlap with other medical conditions. During the diagnostic process, a healthcare provider will conduct a thorough medical history review, looking for any potential risk factors or underlying conditions that may contribute to vagus nerve dysfunction.
In addition to the medical history, a physical examination will be performed to assess any visible signs or abnormalities. However, since the vagus nerve is not easily accessible, further tests are often necessary to confirm the diagnosis. These tests may include electrocardiograms (ECGs), imaging studies, and nerve conduction studies.
Electrocardiograms can help identify any irregularities in heart rhythm, which can be a common symptom of vagus nerve disorders. Imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, can provide detailed images of the structures surrounding the vagus nerve, helping to identify any potential sources of compression or damage. Nerve conduction studies involve measuring the electrical activity of the nerve, providing valuable information about its functionality and potential disruptions.
By combining the information gathered from the medical history, physical examination, and diagnostic tests, healthcare professionals can accurately diagnose vagus nerve disorders and develop an appropriate treatment plan.
Treatment Options for Vagus Nerve Disorders
The treatment of vagus nerve disorders largely depends on the specific condition and its severity. In some cases, lifestyle modifications such as stress reduction techniques, dietary changes, and regular exercise can alleviate symptoms. Stress reduction techniques, such as deep breathing exercises and meditation, can help calm the nervous system and promote vagus nerve function. Dietary changes, such as avoiding trigger foods or consuming foods rich in nutrients that support nerve health, may also be beneficial.
Medications may be prescribed to manage symptoms and regulate the functioning of the vagus nerve. These medications can include pain relievers, anti-inflammatory drugs, or medications that target specific symptoms, such as antiemetics for nausea or anticholinergics for excessive sweating.
In more severe cases, surgical interventions such as vagus nerve stimulation or nerve decompression surgery may be considered. Vagus nerve stimulation involves the implantation of a device that delivers electrical signals to the nerve, helping to regulate its activity. This technique has shown promising results in the management of certain conditions, such as epilepsy and treatment-resistant depression.
Nerve decompression surgery aims to relieve pressure or tension on the nerve, often providing relief from symptoms. This procedure involves identifying and addressing any structures or tissues that may be compressing or irritating the vagus nerve. It is a delicate surgery that requires the expertise of a skilled surgeon.
Overall, the treatment approach for vagus nerve disorders is individualized, taking into account the specific condition, its severity, and the patient’s overall health. Collaborating with healthcare professionals, patients can explore various treatment options and make informed decisions to improve their quality of life.
The Impact of Vagus Nerve Disorders on Daily Life
Vagus nerve disorders can significantly impact an individual’s daily life, affecting physical, emotional, and social well-being. Living with a vagus nerve disorder requires individuals to navigate various challenges and make adjustments to accommodate their condition.
One of the physical impacts of vagus nerve disorders is the potential limitation in the ability to engage in certain activities. For example, individuals may experience difficulties with swallowing or speaking, which can affect their ability to eat or communicate effectively. These challenges can lead to frustration and a sense of isolation.
Furthermore, the unpredictable nature of symptoms can also impact interpersonal relationships and social interactions. Individuals with vagus nerve disorders may have to cancel plans last minute or decline invitations due to sudden flare-ups or symptoms. This can strain relationships and make it challenging to maintain a consistent social life.
Living with a Vagus Nerve Disorder
Living with a vagus nerve disorder can be a complex journey. It requires individuals to adapt and find ways to optimize their daily functioning despite the challenges they face. This may involve making lifestyle changes, such as modifying their diet or incorporating regular exercise to manage symptoms.
In addition to physical adjustments, individuals with vagus nerve disorders may also need to prioritize self-care and emotional well-being. The impact of the condition on mental health can be significant, with individuals experiencing feelings of anxiety, depression, or frustration. Seeking therapy or counseling can provide a safe space to explore these emotions and develop coping mechanisms.
Coping Strategies and Support for Patients
Support networks and coping strategies are crucial for individuals managing vagus nerve disorders. Connecting with other individuals facing similar challenges through support groups or online communities can provide valuable insights and emotional support. Sharing experiences and learning from others who have found effective ways to manage their condition can be empowering.
Developing coping strategies such as relaxation techniques, mindfulness practices, and stress management can also help individuals navigate the impact of their condition on daily life. Engaging in activities that promote relaxation, such as yoga or meditation, can help reduce stress levels and improve overall well-being. Additionally, seeking support from healthcare professionals who specialize in vagus nerve disorders can provide guidance on managing symptoms and optimizing daily functioning.
It is important to remember that each individual’s experience with vagus nerve disorders is unique. What works for one person may not work for another. Therefore, it is crucial for individuals to explore different strategies and approaches to find what best suits their needs and enhances their quality of life.
Advances in Vagus Nerve Disorder Research
Research into vagus nerve disorders is continually evolving, aiming to unravel the complexities surrounding their diagnosis and treatment. Insights gained from ongoing studies and breakthroughs hold promising prospects for improved understanding and management of these disorders.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and inflammation. When this nerve becomes dysfunctional or damaged, it can lead to a range of disorders, such as gastroparesis, epilepsy, depression, and chronic pain.
Current Research and Future Directions
Ongoing research focuses on exploring novel diagnostic techniques, refining the understanding of the underlying mechanisms of vagus nerve disorders, and developing targeted therapies. This includes investigating the role of inflammation, neural circuitry, and genetics in the development and progression of these disorders. By unraveling the intricate interplay between these factors, researchers hope to identify new biomarkers and potential therapeutic targets.
One area of interest is the gut-brain axis, which highlights the bidirectional communication between the gut and the brain through the vagus nerve. Researchers are investigating how disruptions in this communication may contribute to the development of vagus nerve disorders. By understanding these complex interactions, scientists aim to develop innovative interventions that restore the balance and function of the vagus nerve.
Advancements in technology have also revolutionized the field of vagus nerve disorder research. Sophisticated imaging techniques, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), allow researchers to visualize the activity of the vagus nerve and its associated brain regions. This provides valuable insights into the neural pathways involved in vagus nerve disorders and aids in the development of targeted therapies.
Potential Breakthroughs in Vagus Nerve Disorder Treatment
Exciting breakthroughs in vagus nerve disorder treatment are on the horizon. Researchers are exploring the potential of bioelectronic medicine, utilizing implants and devices to modulate the vagus nerve’s activity. These innovative approaches hold promise in providing more personalized and effective treatment options for individuals affected by vagus nerve disorders.
One such technique is vagus nerve stimulation (VNS), which involves implanting a small device that delivers electrical impulses to the vagus nerve. This therapy has shown promising results in the management of epilepsy and depression, with some patients experiencing significant reductions in seizure frequency and improved mood.
Another emerging area of research is the use of transcutaneous vagus nerve stimulation (tVNS), a non-invasive technique that involves applying electrical stimulation to the skin overlying the vagus nerve. Preliminary studies suggest that tVNS may have potential therapeutic benefits for various conditions, including migraine, fibromyalgia, and inflammatory bowel disease.
Furthermore, advancements in neurostimulation techniques, such as closed-loop systems, are being explored. These systems use real-time feedback to adjust the stimulation parameters based on the individual’s physiological responses, optimizing the therapeutic effects and minimizing side effects.
In conclusion, disorders involving the vagus nerve can have a significant impact on various bodily functions, overall well-being, and daily life. By deepening our understanding of the anatomy, function, and common disorders associated with the vagus nerve, healthcare professionals and researchers can work towards improved diagnosis, treatment, and support for affected individuals. Ongoing advancements in research pave the way for a brighter future, offering hope for enhanced management and a higher quality of life for those living with vagus nerve disorders.