The vagus nerve is a crucial component of the body’s autonomic nervous system, responsible for regulating various bodily functions. Disorders involving the vagus nerve can cause a wide range of symptoms and have significant implications for affected individuals. Understanding the anatomy, function, and role of the vagus nerve is essential in comprehending these disorders and their underlying causes.
Understanding the Vagus Nerve
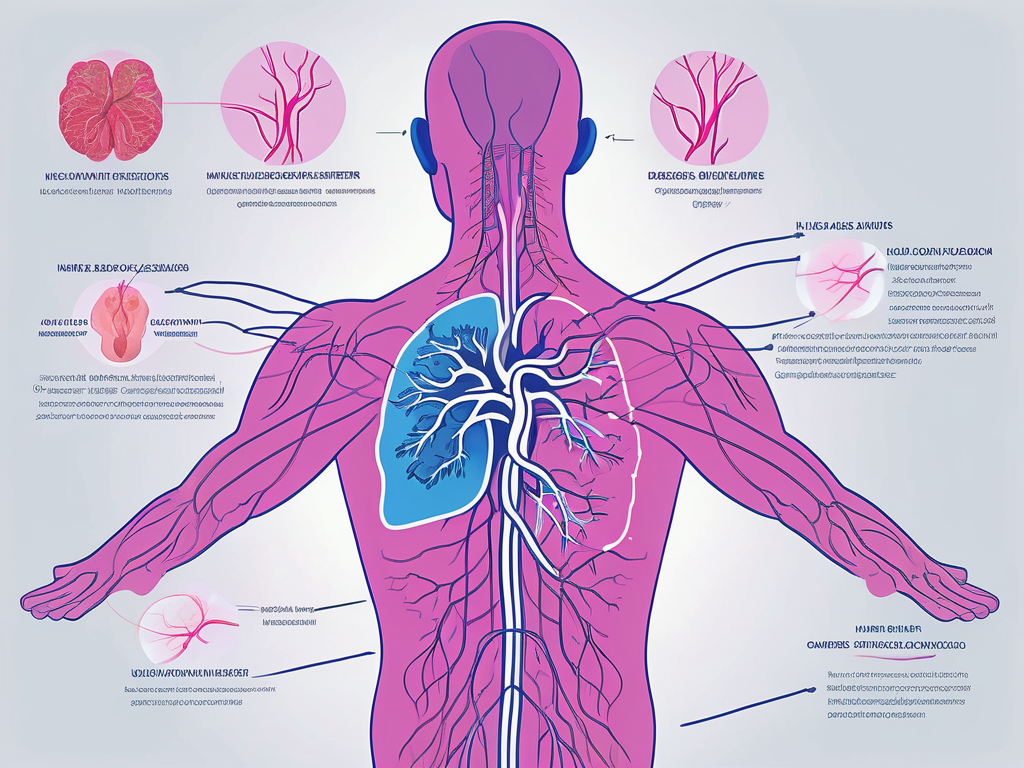
The vagus nerve, also known as the tenth cranial nerve or CN X, is one of the longest and most complex nerves in the body. It consists of a pair of nerves that originate from the medulla oblongata in the brainstem and branch out to various organs and tissues in the body. This cranial nerve plays a vital role in the parasympathetic nervous system, which governs involuntary bodily functions such as digestion, breathing, and heart rate.
Anatomy and Function of the Vagus Nerve
The vagus nerve is comprised of both motor and sensory fibers, allowing it to transmit information to and from the brain. Its motor fibers control movements in the throat, tongue, and facial muscles, while its sensory fibers relay sensations from the throat, heart, lungs, and abdominal organs. This bidirectional communication enables the vagus nerve to regulate numerous bodily functions and maintain homeostasis.
The vagus nerve delivers parasympathetic signals to the heart, slowing the heart rate, reducing blood pressure, and promoting relaxation. It also stimulates digestion by increasing the production of stomach acids and digestive enzymes and enhancing intestinal motility. Additionally, the vagus nerve influences lung function, promoting bronchoconstriction and an increase in mucus production.
Role of the Vagus Nerve in the Body
Beyond its role in autonomic regulation, the vagus nerve plays a crucial role in modulating the body’s stress response. It exerts an anti-inflammatory effect through the release of acetylcholine, which inhibits the production of pro-inflammatory molecules. This anti-inflammatory pathway, known as the cholinergic anti-inflammatory pathway, helps prevent excessive inflammation and maintain immune balance.
Furthermore, the vagus nerve is intricately involved in the gut-brain axis, which represents the bidirectional communication between the gut and the brain. The vagus nerve facilitates the transmission of signals between the gut and the brain, influencing mood, cognition, and behavior. This connection underscores the potential impact of vagus nerve disorders on mental health and overall well-being.
Moreover, recent research has shed light on the role of the vagus nerve in regulating appetite and weight. Studies have shown that vagus nerve stimulation can lead to weight loss by reducing appetite and increasing feelings of fullness. This discovery has opened up new possibilities for the treatment of obesity and related metabolic disorders.
In addition to its influence on bodily functions, the vagus nerve also plays a role in social bonding and empathy. Research has shown that stimulating the vagus nerve can enhance social behavior and increase feelings of empathy and compassion. This suggests that the vagus nerve may be involved in the complex interplay between our nervous system and our social interactions.
Furthermore, the vagus nerve has been implicated in the regulation of sleep. Studies have found that vagus nerve activity is closely linked to the different stages of sleep, with increased activity during deep sleep and decreased activity during REM sleep. This suggests that the vagus nerve may play a role in the restorative functions of sleep and the regulation of sleep-wake cycles.
Overall, the vagus nerve is a fascinating and multifaceted component of the human body. Its intricate connections and wide-ranging effects highlight its importance in maintaining physiological balance and overall well-being. Further research into the vagus nerve promises to uncover even more intriguing insights into its functions and potential therapeutic applications.
Disorders Associated with the Vagus Nerve
Disorders involving the vagus nerve can manifest in various ways, depending on the affected area and the extent of nerve dysfunction. Common symptoms and signs may include difficulty swallowing (dysphagia), hoarseness, voice changes, heart palpitations, gastrointestinal disturbances, and even mood alterations.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in the functioning of many organs and systems in the body. It is the longest cranial nerve, extending from the brainstem to the abdomen, and is responsible for regulating a wide range of bodily functions. When this nerve is affected by disorders, it can have significant implications on a person’s overall health and well-being.
Common Symptoms and Signs
Dysphagia, characterized by difficulty swallowing or a sensation of food getting stuck in the throat, can result from vagus nerve damage affecting the muscles involved in swallowing. This can make it challenging for individuals to enjoy meals and may lead to unintended weight loss or malnutrition if left untreated.
Hoarseness or changes in voice quality can occur due to impaired vocal cord movement. The vagus nerve innervates the muscles responsible for controlling the vocal cords, and any dysfunction in this nerve can lead to voice changes or even complete loss of voice. This can have a profound impact on an individual’s ability to communicate effectively and may require speech therapy or other interventions to improve vocal function.
Heart palpitations and irregular heart rhythms may arise if vagus nerve dysfunction disrupts the heart’s normal regulatory mechanisms. The vagus nerve helps to maintain a balance between the sympathetic and parasympathetic nervous systems, which control heart rate and blood pressure. When this balance is disrupted, it can result in palpitations, rapid heart rate, or even more serious cardiac arrhythmias.
Gastrointestinal disturbances such as nausea, vomiting, abdominal pain, and bloating may indicate vagus nerve involvement. These symptoms can arise as a result of impaired motility and altered digestive secretions. The vagus nerve plays a crucial role in coordinating the movement of food through the digestive tract and stimulating the release of digestive enzymes. When this nerve is not functioning properly, it can lead to delayed gastric emptying (gastroparesis) and other gastrointestinal issues.
Furthermore, vagus nerve disorders have been associated with mood disorders such as anxiety and depression, emphasizing the influence of this nerve on mental well-being. The vagus nerve is involved in the regulation of the autonomic nervous system, which controls many involuntary bodily functions, including mood and emotions. When the vagus nerve is affected, it can disrupt the delicate balance of neurotransmitters in the brain, leading to mood alterations and mental health issues.
Specific Disorders and Their Implications
Specific disorders involving the vagus nerve include vocal cord paralysis, gastroparesis, neurogenic bowel, and vasovagal syncope. Vocal cord paralysis causes hoarseness and difficulty speaking, impacting communication and reducing the quality of life for affected individuals. It can be caused by damage to the vagus nerve or its branches, leading to impaired movement of the vocal cords. Treatment options for vocal cord paralysis may include voice therapy, surgical interventions, or the use of vocal cord implants to restore voice function.
Gastroparesis refers to delayed gastric emptying, leading to symptoms such as bloating, nausea, and vomiting. The vagus nerve plays a crucial role in coordinating the movement of food through the stomach and intestines. When this nerve is damaged or not functioning properly, it can result in a slowed or disrupted digestive process. Treatment for gastroparesis may involve dietary modifications, medications to improve gastric motility, and in severe cases, surgical interventions.
Neurogenic bowel can result in constipation or fecal incontinence. The vagus nerve helps to regulate the movement of the intestines and the release of stool. When this nerve is damaged, it can lead to a loss of bowel control or difficulty with bowel movements. Management of neurogenic bowel may involve dietary changes, medications, and the use of bowel management techniques to promote regularity and prevent complications.
Vasovagal syncope is characterized by a sudden drop in blood pressure and fainting spells. The vagus nerve plays a role in regulating blood pressure and heart rate, and dysfunction in this nerve can result in episodes of syncope. Triggers for vasovagal syncope can vary from person to person and may include emotional stress, pain, or even prolonged standing. Treatment options for vasovagal syncope may include lifestyle modifications, medications to stabilize blood pressure, and in some cases, the use of a pacemaker to regulate heart rate.
Causes of Vagus Nerve Disorders
Vagus nerve disorders can arise from various factors, including genetic factors and environmental triggers. Understanding these underlying causes is crucial in diagnosing and managing these conditions effectively.
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in the functioning of the body. It is responsible for controlling various bodily functions, such as heart rate, digestion, and even mood. When the vagus nerve is disrupted or damaged, it can lead to a range of symptoms and health issues.
Genetic Factors
Genetic mutations can predispose individuals to develop vagus nerve disorders. These mutations can affect the development, structure, or function of the vagus nerve, leading to dysfunction and associated symptoms. In some cases, these genetic mutations may be inherited from one or both parents, increasing the likelihood of developing a vagus nerve disorder.
Researchers have identified several specific gene mutations that are associated with vagus nerve disorders. For example, mutations in the SCN10A gene have been linked to conditions such as familial dysautonomia, a rare genetic disorder that affects the autonomic nervous system, including the vagus nerve. Understanding the genetic basis of vagus nerve disorders can help in early diagnosis and targeted treatment approaches.
Genetic counseling and testing may be beneficial in identifying individuals at risk and implementing appropriate management strategies. By identifying specific genetic mutations, healthcare providers can offer personalized treatment plans and interventions to manage symptoms and improve the quality of life for individuals with vagus nerve disorders.
Environmental Triggers
Environmental factors can also contribute to the development of vagus nerve disorders. Infections, physical trauma, autoimmune conditions, and exposure to toxins or certain medications can all impact the health and functioning of the vagus nerve. These triggers can cause inflammation, damage, or disruption to the nerve, leading to a range of symptoms and complications.
Infections, such as Lyme disease or viral infections, can directly affect the vagus nerve, leading to inflammation and dysfunction. Physical trauma, such as a car accident or sports injury, can also damage the vagus nerve, resulting in symptoms like difficulty swallowing, voice changes, or irregular heart rhythms.
Autoimmune conditions, such as multiple sclerosis or Guillain-Barré syndrome, can cause the immune system to mistakenly attack the vagus nerve, leading to nerve damage and dysfunction. Additionally, exposure to certain toxins, such as heavy metals or industrial chemicals, can have a detrimental effect on the vagus nerve, impairing its ability to transmit signals effectively.
Identifying and minimizing exposure to these triggers can help prevent or manage vagus nerve disorders more effectively. For example, practicing good hygiene and taking precautions to avoid infections can reduce the risk of developing vagus nerve-related complications. Similarly, taking steps to reduce exposure to toxins and maintaining a healthy lifestyle can support the overall health and functioning of the vagus nerve.
In conclusion, vagus nerve disorders can be caused by a combination of genetic factors and environmental triggers. Genetic mutations can predispose individuals to develop these disorders, while infections, physical trauma, autoimmune conditions, and exposure to toxins can also contribute to their development. Understanding these underlying causes is essential in diagnosing and managing vagus nerve disorders effectively, allowing for personalized treatment approaches and improved quality of life.
Diagnosing Vagus Nerve Disorders
Diagnosing vagus nerve disorders involves a comprehensive evaluation, considering both medical history and physical examination findings, alongside specific diagnostic tests and procedures.
Medical History and Physical Examination
A detailed medical history, including the onset and progression of symptoms, any underlying conditions, and a family history of neurological disorders, is crucial in reaching an accurate diagnosis. During the physical examination, healthcare professionals assess vital signs, cranial nerve function, and perform specific tests to evaluate the involvement of the vagus nerve.
Diagnostic Tests and Procedures
Various tests and procedures can aid in the diagnosis of vagus nerve disorders. These may include electromyography (EMG) to assess muscle function, endoscopic evaluations to evaluate vocal cord movement and gastrointestinal motility, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to visualize nerve abnormalities or structural changes, and autonomic function tests to evaluate nerve function and autonomic regulation.
Treatment Options for Vagus Nerve Disorders
Treatment options for vagus nerve disorders aim to manage symptoms, improve quality of life, and address any underlying causes.
Medications and Therapies
Pharmacological interventions may include medications to manage specific symptoms, such as proton pump inhibitors for gastroparesis or antidepressants for mood disorders. Physical therapy can help improve muscle function and coordination, while speech therapy may be beneficial for individuals with vocal cord paralysis. Additionally, complementary therapies like biofeedback, acupuncture, and relaxation techniques may provide symptomatic relief and enhance overall well-being.
Surgical Interventions
In severe cases or when conservative treatments fail to provide adequate relief, surgical interventions may be considered. Procedures such as vocal cord injections or surgical reinnervation can restore vocal cord function and improve voice quality. Gastric electrical stimulation or surgical options may be explored for individuals with significant gastrointestinal symptoms. Surgical management should be individually tailored, considering the specific vagus nerve disorder and the patient’s overall health status.
Conclusion
Disorders involving the vagus nerve can have significant implications on an individual’s physical and emotional well-being. Understanding the complex anatomy, function, and role of the vagus nerve is vital in comprehending the causes and implications of these disorders. Genetic factors and environmental triggers play a significant role, while accurate diagnosis and management require a comprehensive approach, considering medical history, physical examination findings, and specific diagnostic tests. Treatment options vary, ranging from medications and therapies to surgical interventions, with a focus on symptom management and addressing underlying causes. Continued research and advancements in understanding vagus nerve disorders hold promise for improved diagnosis, treatment, and ultimately, the overall well-being of affected individuals.