The human body is a complex network of organs and systems, each with its own unique functions and responsibilities. One vital component of this intricate system is the vagus nerve, a long, meandering nerve that originates in the brainstem and extends all the way down to the abdomen. While the vagus nerve plays a crucial role in various bodily functions, it has a particularly important role in digestion and the regulation of stomach acid levels.
Understanding the Vagus Nerve and Its Functions
The vagus nerve, also known as the tenth cranial nerve, is one of the longest nerves in the body. It serves as a communication pathway between the brain and various organs, including the heart, lungs, and digestive system. This nerve controls numerous functions, such as heart rate, breathing, sweating, and muscle movements in the gastrointestinal tract.
But what exactly is the vagus nerve and how does it work? Let’s delve deeper into its anatomy and explore its role in digestion.
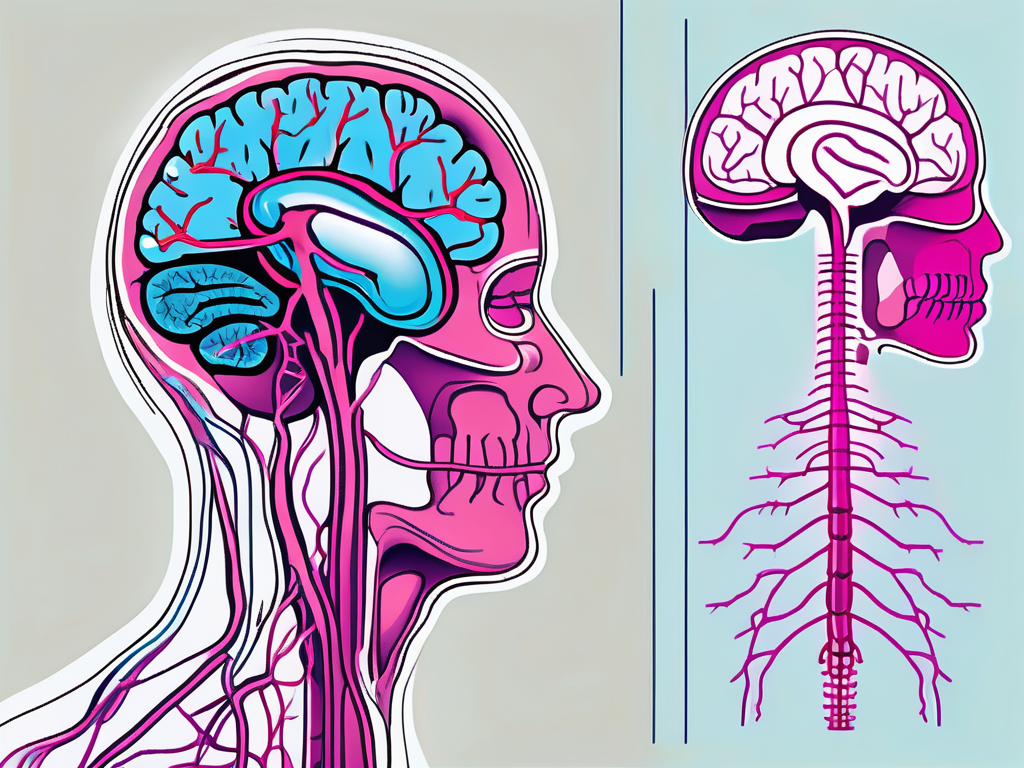
Anatomy of the Vagus Nerve
The vagus nerve is a bundle of nerve fibers that originate in the medulla oblongata, a part of the brainstem. It then travels down through the neck, chest, and abdomen, branching out into multiple smaller nerves that innervate various organs and tissues along the way. This extensive network allows the vagus nerve to relay important signals and information between the brain and the rest of the body.
Within this intricate network, the vagus nerve consists of both sensory and motor fibers. The sensory fibers transmit information from the organs back to the brain, providing feedback on their functioning. On the other hand, the motor fibers carry signals from the brain to the organs, enabling the brain to control their activities.
Furthermore, the vagus nerve is not limited to its role in the digestive system. It also influences other bodily functions, such as heart rate, blood pressure, and even mood regulation. This highlights the widespread impact of the vagus nerve on overall health and well-being.
Role of the Vagus Nerve in Digestion
In the realm of digestion, the vagus nerve plays a crucial role in coordinating the intricate process of breaking down food and absorbing nutrients. It stimulates the secretion of digestive juices, regulates stomach emptying, and controls the contraction and relaxation of the muscles in the gastrointestinal tract.
When you take a bite of food, the vagus nerve immediately gets to work. It sends signals to the stomach, triggering the release of gastric acid and enzymes necessary for digestion. Simultaneously, it communicates with the muscles in the stomach and intestines, ensuring the smooth movement of food along the digestive tract.
Moreover, the vagus nerve acts as a key mediator of the brain-gut axis, which is the bidirectional communication between the brain and the gut. This means that not only does the brain influence digestion through the vagus nerve, but the gut can also send signals back to the brain, affecting our mood and overall well-being.
Research has shown that the vagus nerve is involved in the regulation of appetite and satiety, as well as the modulation of gut inflammation. It also plays a role in the gut-brain connection, influencing mental health conditions such as anxiety and depression. This highlights the intricate relationship between the vagus nerve and our overall digestive and emotional well-being.
In conclusion, the vagus nerve is a remarkable part of our nervous system that connects the brain to various organs, including the heart, lungs, and digestive system. Its extensive network allows for the coordination of essential functions, such as digestion. Understanding the anatomy and functions of the vagus nerve provides valuable insights into the complex interplay between our brain and body.
Vagus Nerve Disorders: An Overview
While the vagus nerve is a remarkable component of our nervous system, it is not immune to disorders and dysfunctions. Vagus nerve disorders can arise from various causes, ranging from trauma or injury to underlying medical conditions. These disorders can lead to a disruption in the normal functioning of this vital nerve, with potential implications for digestion and stomach acid regulation.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and even mood. However, when this intricate system encounters problems, it can result in a range of disorders that require careful diagnosis and management.
Common Vagus Nerve Disorders
There are several known vagus nerve disorders, each with its own set of symptoms and characteristics. One common disorder is called vagus nerve neuropathy, which refers to damage or dysfunction of the nerve. This condition can occur due to trauma, such as a car accident or surgical procedure, or as a result of an underlying medical condition, such as diabetes or autoimmune disorders.
Gastroparesis is another vagus nerve disorder that affects the normal motility of the digestive system. In this condition, the muscles in the stomach do not function properly, leading to delayed emptying of food from the stomach into the small intestine. This can cause symptoms such as bloating, nausea, vomiting, and a feeling of fullness even after eating small amounts of food.
Postoperative ileus is yet another disorder that can affect the vagus nerve. It is a temporary condition that occurs after abdominal surgery, where the normal movement of the intestines is disrupted. This can result in abdominal pain, bloating, constipation, and a lack of appetite.
Symptoms and Diagnosis of Vagus Nerve Disorders
The symptoms of vagus nerve disorders can vary depending on the underlying cause and the specific nerves affected. Common symptoms include difficulty swallowing, heartburn, bloating, nausea, and vomiting. Additionally, individuals with vagus nerve disorders may experience changes in heart rate and blood pressure due to the vagus nerve’s role in regulating these functions.
Diagnosing vagus nerve disorders can be challenging, as the symptoms may overlap with other gastrointestinal conditions. However, medical professionals may perform various tests to assess the function and integrity of the vagus nerve and identify any potential abnormalities. Esophageal manometry is a test that measures the strength and coordination of the muscles in the esophagus. Gastric emptying studies can evaluate the rate at which food leaves the stomach. Imaging scans, such as ultrasound or magnetic resonance imaging (MRI), can provide detailed images of the vagus nerve and surrounding structures.
It is important to note that vagus nerve disorders can have a significant impact on an individual’s quality of life. They can cause chronic pain, discomfort, and disruption of daily activities. Therefore, early diagnosis and appropriate management are essential in order to alleviate symptoms and improve overall well-being.
The Connection Between Vagus Nerve Disorders and Stomach Acid
One significant consequence of vagus nerve disorders is their impact on stomach acid levels. The vagus nerve plays a critical role in regulating the production of stomach acid, which is essential for efficient digestion. Therefore, any dysfunction or disruption in the vagus nerve can lead to decreased stomach acid levels, ultimately affecting the body’s ability to break down and absorb nutrients from food.
The Vagus Nerve’s Role in Stomach Acid Production
Under normal conditions, the vagus nerve stimulates the release of gastric acid or stomach acid by activating the parietal cells in the stomach lining. These cells are responsible for producing hydrochloric acid, a potent acid required for the breakdown of proteins, activation of digestive enzymes, and protection against harmful bacteria that may enter the digestive system through food.
When food enters the stomach, the vagus nerve sends signals to the parietal cells, triggering the release of hydrochloric acid. This acid creates an acidic environment in the stomach, which is necessary for the proper digestion of food. It helps to denature proteins, making them more accessible to digestive enzymes, and also kills off any bacteria or pathogens that may be present in the food.
Furthermore, the vagus nerve also stimulates the release of other substances, such as pepsinogen, which is converted into the enzyme pepsin. Pepsin plays a crucial role in breaking down proteins into smaller peptides, facilitating their absorption in the small intestine.
How Vagus Nerve Disorders Affect Stomach Acid Levels
When the vagus nerve is not functioning properly due to a disorder or dysfunction, the signals that stimulate the release of stomach acid may become impaired. As a result, the production of stomach acid decreases, leading to a condition known as hypochlorhydria, which is characterized by low stomach acid levels.
Hypochlorhydria can have significant implications for digestion and overall health. Insufficient stomach acid can hinder the breakdown of food, impair the absorption of nutrients, and increase the risk of bacterial overgrowth in the gastrointestinal tract. Moreover, low stomach acid levels can contribute to symptoms such as indigestion, heartburn, and nutrient deficiencies.
In addition to its impact on digestion, the vagus nerve is also involved in regulating other bodily functions, including heart rate, breathing, and the release of various hormones. Therefore, vagus nerve disorders can have far-reaching effects beyond stomach acid production.
It is important to note that vagus nerve disorders can have different causes, ranging from autoimmune conditions to physical damage or compression of the nerve. Identifying the underlying cause of the disorder is crucial for developing an appropriate treatment plan.
Treatment options for vagus nerve disorders may include medications to manage symptoms, physical therapy to improve nerve function, and in some cases, surgical interventions to address any structural issues affecting the nerve. Additionally, lifestyle modifications such as stress reduction techniques, dietary changes, and regular exercise may also play a role in managing vagus nerve disorders and their impact on stomach acid levels.
In conclusion, the connection between vagus nerve disorders and stomach acid levels is a complex and important one. The vagus nerve’s role in stimulating the release of stomach acid is crucial for efficient digestion and nutrient absorption. When the vagus nerve is not functioning properly, as is the case with vagus nerve disorders, stomach acid production can be significantly affected, leading to various digestive issues and potential nutrient deficiencies. Understanding this connection is essential for diagnosing and managing vagus nerve disorders effectively.
Health Implications of Decreased Stomach Acid
When stomach acid levels are consistently low due to vagus nerve disorders or hypochlorhydria, it can have far-reaching consequences for an individual’s health and well-being. Proper stomach acid levels are essential for several aspects of digestion and nutrient absorption, and their deficiency can lead to various health risks.
Understanding Hypochlorhydria
Hypochlorhydria, or low stomach acid, is a condition that can occur as a result of vagus nerve disorders or other underlying factors. It is often associated with symptoms such as bloating, belching, gas, and abdominal discomfort. Individuals with hypochlorhydria may also experience a decrease in gastric enzyme secretion and a compromised ability to absorb certain vitamins and minerals, including iron, calcium, and vitamin B12.
Health Risks Associated with Low Stomach Acid
Low stomach acid levels not only interfere with the breakdown of food and absorption of nutrients but also increase the risk of gastrointestinal infections. Stomach acid provides a protective barrier against harmful bacteria and other pathogens that may enter the digestive system. When the acid levels are low, the body becomes more vulnerable to these microorganisms, potentially leading to infections and related health complications.
In addition, low stomach acid can contribute to the development of other digestive disorders, such as small intestinal bacterial overgrowth (SIBO), as the reduced acidity provides an environment conducive to bacterial proliferation in the small intestine. This, in turn, can lead to symptoms such as bloating, diarrhea, and malabsorption.
Treatment and Management of Vagus Nerve Disorders
While vagus nerve disorders can present significant challenges, there are various treatment options and management strategies available to help individuals cope with and alleviate their symptoms.
Medical Treatments for Vagus Nerve Disorders
Depending on the specific vagus nerve disorder and its underlying cause, healthcare professionals may prescribe medications or therapies to manage the condition. For example, medications that enhance the motility of the gastrointestinal tract, such as prokinetic agents, can help alleviate symptoms of gastroparesis, a disorder that affects the vagus nerve’s ability to regulate stomach emptying.
In severe cases or when conservative measures fail, surgical interventions may be considered. Surgical options, such as vagotomy or nerve stimulation devices, aim to modulate the function of the vagus nerve and restore the normal communication between the brain and the digestive system.
Lifestyle Changes to Improve Vagus Nerve Health
In addition to medical treatments, certain lifestyle changes and self-care practices can contribute to the overall health and well-being of the vagus nerve. These include stress management techniques, regular exercise, a balanced diet rich in nutrients, and adequate sleep. Engaging in activities that stimulate the vagus nerve, such as deep breathing exercises and yoga, may also help support its proper functioning.
In conclusion, the vagus nerve is a critical component of the nervous system, influencing various bodily functions, including digestion and stomach acid regulation. Vagus nerve disorders can disrupt this complex system, leading to decreased stomach acid levels and subsequent health implications. Understanding the role of the vagus nerve in digestion, recognizing common disorders, and exploring treatment and management options can contribute to better overall health and well-being for those affected by these conditions.