Fainting disorders, also known as syncope, can be distressing and often occur unexpectedly. These disorders have been linked to the vagus nerve, a vital component of the autonomic nervous system responsible for regulating various bodily functions. To gain a better understanding of these disorders and their connection to the vagus nerve, it is essential to delve into the anatomy and functions of this remarkable nerve.
The Anatomy of the Vagus Nerve
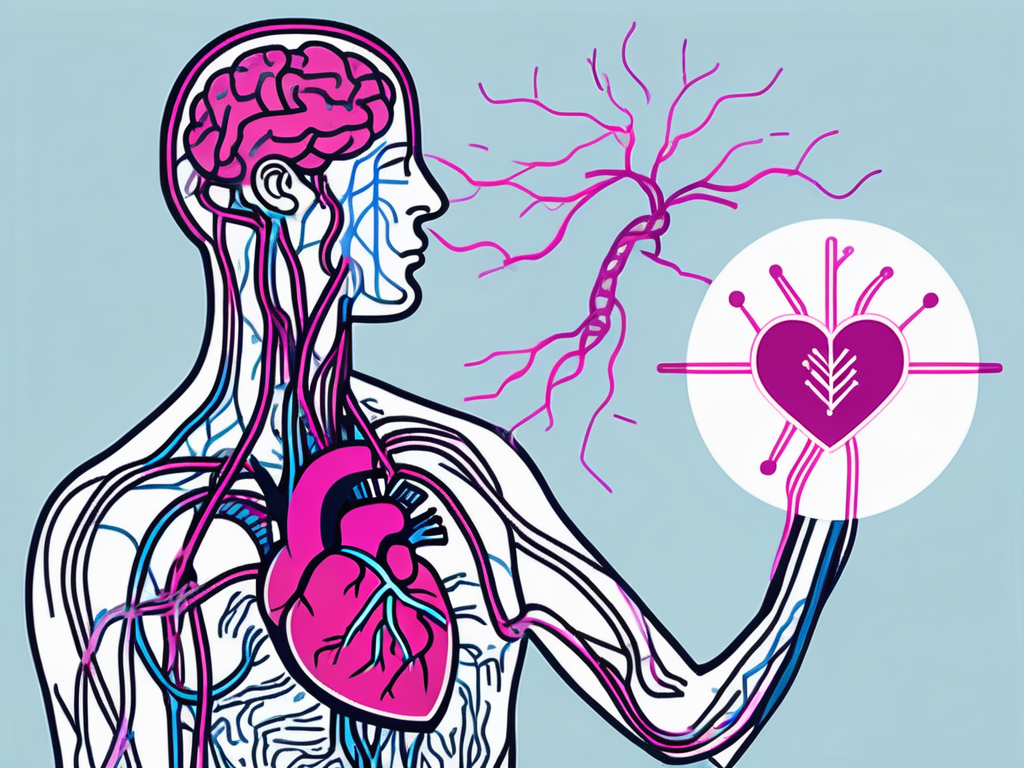
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most complex nerves in the body. Originating in the brainstem, it extends downward, connecting to various organs and structures in the neck, chest, and abdomen. Comprising both motor and sensory fibers, the vagus nerve plays a crucial role in regulating many bodily functions.
As the vagus nerve travels through the body, it branches out extensively, forming intricate networks of nerve fibers. These fibers innervate organs such as the heart, lungs, liver, stomach, and intestines, allowing for precise control and coordination of their functions. The vagus nerve acts as a communication highway, transmitting signals between the brain and these vital organs.
Role and Function of the Vagus Nerve
The vagus nerve serves as a vital component of the parasympathetic division of the autonomic nervous system. It regulates involuntary bodily processes such as heart rate, respiration, digestion, and glandular secretion. When the body is in a state of relaxation, the vagus nerve promotes a calm and restful state by slowing down the heart rate, reducing blood pressure, and facilitating efficient digestion.
Furthermore, the vagus nerve is involved in the control of swallowing and speech. It coordinates the intricate movements of the muscles involved in these processes, ensuring smooth and efficient actions. Additionally, the vagus nerve plays a role in various sensory functions in the head and neck region, including taste, touch, and temperature sensation.
The Vagus Nerve and the Autonomic Nervous System
The autonomic nervous system consists of two branches: the sympathetic and parasympathetic. While the sympathetic branch is responsible for the “fight or flight” response, the parasympathetic branch, with the vagus nerve as its primary component, promotes the “rest and digest” response. The vagus nerve modulates the functions of organs and glands, maintaining a delicate balance to ensure homeostasis.
When the body is under stress or in a threatening situation, the sympathetic branch of the autonomic nervous system becomes activated, leading to increased heart rate, rapid breathing, and heightened alertness. However, once the threat has passed, the vagus nerve kicks in, counteracting the sympathetic response and restoring the body to a state of calmness and relaxation.
Moreover, the vagus nerve plays a crucial role in the regulation of inflammation. It has anti-inflammatory effects and can help dampen the body’s immune response. This ability is particularly important in preventing excessive inflammation, which can contribute to various chronic diseases.
In conclusion, the vagus nerve is a remarkable structure that connects the brain to vital organs and plays a crucial role in regulating numerous bodily functions. Its intricate network of fibers allows for precise control and coordination, ensuring the smooth functioning of the parasympathetic division of the autonomic nervous system. Understanding the anatomy and function of the vagus nerve provides valuable insights into the complex mechanisms that maintain our overall health and well-being.
Fainting Disorders: An Overview
Fainting disorders, also known as syncope, refer to a temporary loss of consciousness due to a sudden decrease in blood flow to the brain. This can be a frightening experience for those who have experienced it, and understanding the different types of fainting disorders can help shed light on their causes and potential treatments.
Defining fainting disorders is essential in order to grasp the underlying mechanisms that lead to this loss of consciousness. Fainting occurs when there is inadequate blood supply or oxygen delivery to the brain. This can be caused by a multitude of factors, ranging from sudden changes in position to intense emotions, pain, dehydration, medications, or underlying medical conditions.
One of the most common types of fainting disorders is vasovagal syncope. This type of syncope is primarily mediated by the vagus nerve, which plays a crucial role in regulating heart rate and blood pressure. When the vagus nerve is overstimulated, it can lead to a sudden drop in heart rate and blood pressure, resulting in fainting. Interestingly, vasovagal syncope is often triggered by certain stimuli, such as the sight of blood, extreme pain, or even prolonged standing.
Another type of fainting disorder is neurological syncope. This occurs when there is a disruption in the normal functioning of the brain, leading to a loss of consciousness. Neurological syncope can be caused by various factors, including seizures, migraines, or even certain medications that affect the central nervous system.
Cardiac syncope, on the other hand, is characterized by fainting episodes that are directly related to heart problems. This can include arrhythmias, structural abnormalities of the heart, or even heart attacks. It is crucial to identify and address the underlying cardiac issues to effectively manage and prevent further episodes of syncope.
Orthostatic hypotension is yet another type of fainting disorder that occurs when there is a sudden drop in blood pressure upon standing up. This can happen due to various reasons, such as dehydration, certain medications, or even autonomic nervous system dysfunction. Understanding the triggers and mechanisms behind orthostatic hypotension can help individuals take necessary precautions to prevent fainting episodes.
In conclusion, fainting disorders encompass a range of conditions that can lead to a temporary loss of consciousness. From vasovagal syncope to neurological syncope, cardiac syncope, and orthostatic hypotension, each type has its unique characteristics and triggers. By delving deeper into the intricacies of these disorders, healthcare professionals can provide better care and support to those who experience fainting episodes.
The Connection Between the Vagus Nerve and Fainting Disorders
Understanding the role of the vagus nerve in fainting disorders is crucial in comprehending why these conditions arise and how they can be managed.
How the Vagus Nerve Influences Fainting
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in regulating heart rate and blood pressure. It is the longest and most complex of the cranial nerves, extending from the brainstem to various organs in the body, including the heart, lungs, and digestive system.
When the vagus nerve becomes overactive or excessively stimulated, it can lead to a sudden decrease in heart rate and a drop in blood pressure, resulting in loss of consciousness. This phenomenon is known as vasovagal syncope, a common type of fainting disorder.
During a vasovagal syncope episode, the vagus nerve sends signals to the heart, causing it to slow down and reducing the force with which blood is pumped throughout the body. At the same time, the nerve also triggers the relaxation of blood vessels, leading to a decrease in blood pressure. The combination of reduced heart rate and lowered blood pressure can result in inadequate blood flow to the brain, leading to fainting.
Vagus Nerve Stimulation and Fainting Disorders
Vagus nerve stimulation, a therapeutic technique involving the use of electrical impulses to stimulate the nerve, has shown promise in managing certain types of fainting disorders. This approach aims to modulate the activity of the vagus nerve, helping to regulate heart rate and blood pressure, and reducing the occurrence of syncope episodes.
During vagus nerve stimulation, a small device is implanted under the skin, usually in the chest area. This device is connected to the vagus nerve and delivers mild electrical impulses to the nerve at regular intervals. These impulses help to regulate the nerve’s activity and can prevent it from becoming overactive or excessively stimulated, thereby reducing the risk of fainting.
Studies have shown that vagus nerve stimulation can be particularly effective in managing reflex syncope, a type of fainting disorder triggered by specific stimuli, such as emotional stress or the sight of blood. By modulating the vagus nerve’s response to these triggers, the frequency and severity of reflex syncope episodes can be significantly reduced.
In addition to its potential therapeutic benefits, vagus nerve stimulation also holds promise in the field of research. Scientists are exploring its use in treating various neurological conditions, including epilepsy, depression, and migraine headaches. By further understanding the intricate connections between the vagus nerve and these disorders, researchers hope to develop new and innovative treatment approaches.
In conclusion, the vagus nerve plays a crucial role in regulating heart rate and blood pressure, and its dysfunction can contribute to fainting disorders. Vagus nerve stimulation offers a promising therapeutic approach for managing certain types of fainting disorders, and ongoing research continues to shed light on the intricate connections between the vagus nerve and various neurological conditions.
Symptoms and Diagnosis of Vagus Nerve-Related Fainting Disorders
Recognizing and diagnosing vagus nerve-related fainting disorders are crucial steps in effectively managing these conditions.
Fainting episodes associated with the vagus nerve can manifest with various symptoms, including lightheadedness, dizziness, pale skin, sweating, blurred vision, and a slow or irregular heartbeat. Identifying these warning signs can aid in determining the underlying cause and appropriate treatment approach.
When it comes to diagnosing vagus nerve-related fainting disorders, medical professionals employ a range of diagnostic procedures and tests. These procedures and tests are designed to gather comprehensive information about the patient’s condition, enabling healthcare providers to make accurate diagnoses and develop effective treatment plans.
One of the initial steps in the diagnostic process is the evaluation of the patient’s medical history. By reviewing the patient’s past medical records, doctors can gain insights into any previous fainting episodes, underlying health conditions, and potential triggers. This information is valuable in identifying patterns and establishing a baseline for further investigation.
Physical examinations are another essential component of diagnosing vagus nerve-related fainting disorders. During these examinations, healthcare providers assess the patient’s overall health, looking for any abnormalities or signs of underlying conditions. They may check the patient’s blood pressure, heart rate, and perform neurological tests to evaluate the functioning of the vagus nerve.
Electrocardiograms (ECGs) are commonly used to evaluate heart function in patients experiencing fainting episodes. These tests measure the electrical activity of the heart, providing valuable information about the heart’s rhythm and detecting any irregularities that may be associated with vagus nerve dysfunction.
In some cases, healthcare providers may recommend echocardiograms to further assess the structure and function of the heart. These non-invasive tests use sound waves to create detailed images of the heart, allowing doctors to evaluate its chambers, valves, and overall efficiency.
Tilt-table tests are frequently employed to provoke fainting episodes in a controlled environment. During these tests, patients are secured to a table that can be tilted to different angles. By monitoring the patient’s blood pressure, heart rate, and symptoms while changing positions, healthcare providers can determine if the vagus nerve is playing a role in the fainting episodes.
Holter monitoring, which involves wearing a portable device that continuously records the heart’s electrical activity over a period of 24 to 48 hours, may also be utilized. This extended monitoring allows doctors to capture any irregularities that may occur outside of a clinical setting, providing a more comprehensive picture of the patient’s heart function.
By utilizing a combination of these diagnostic procedures and tests, healthcare providers can gather the necessary information to diagnose vagus nerve-related fainting disorders accurately. Once a diagnosis is made, the most suitable treatment plan can be developed, taking into account the individual needs and circumstances of the patient.
Treatment Options for Fainting Disorders Linked to the Vagus Nerve
Managing fainting disorders linked to the vagus nerve often involves a multi-faceted approach, comprising both medical interventions and lifestyle modifications.
Medications and Therapies
In some cases, medications such as beta-blockers or anticholinergic drugs may be prescribed to regulate heart rate and blood pressure. Additionally, therapies such as vagus nerve stimulation and cardiac pacing can help prevent syncope episodes and improve overall quality of life.
Lifestyle Changes and Home Remedies
Implementing certain lifestyle changes alongside medical interventions can significantly reduce the occurrence of fainting episodes. Strategies may include increasing fluid intake, avoiding triggers, practicing stress-reduction techniques, maintaining adequate rest, and using compression stockings to improve blood circulation.
In conclusion, understanding fainting disorders linked to the vagus nerve is essential for effective management and treatment. By comprehending the anatomy and functions of the vagus nerve, recognizing the symptoms, and exploring treatment options, medical professionals can provide optimal care and enhance the quality of life for individuals experiencing these disorders.