The left vagus nerve is a crucial component of the human body’s autonomic nervous system. It plays a vital role in regulating various bodily functions, such as digestion, heart rate, and breathing. When the left vagus nerve is affected by disorders, it can lead to a range of distressing symptoms and complications.
An Overview of the Vagus Nerve
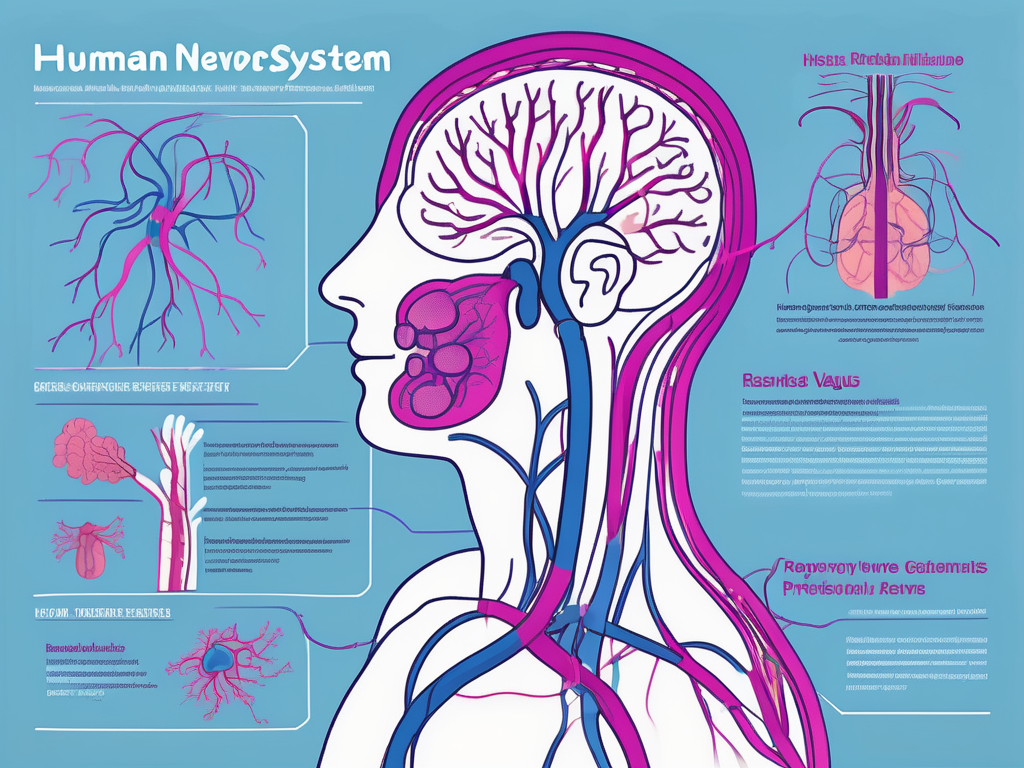
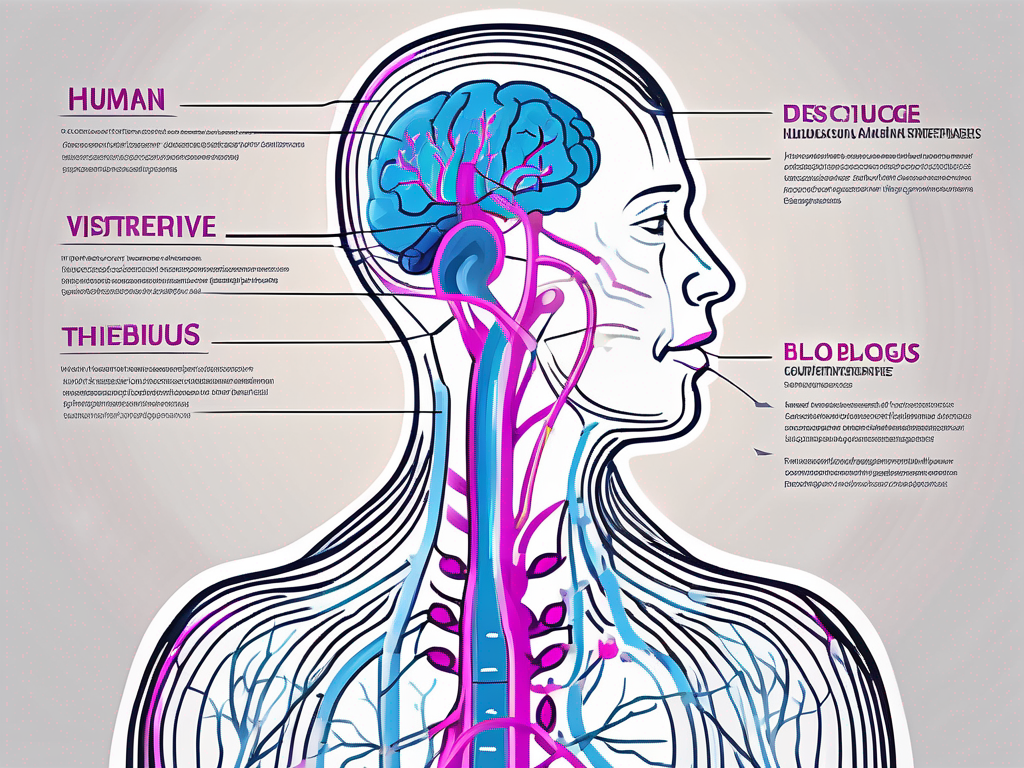
The vagus nerve, also known as the tenth cranial nerve, is one of the longest nerves in the human body. It originates in the medulla oblongata, which is located in the brainstem. The vagus nerve consists of both left and right branches, each with distinct functions and connections throughout the body.
The vagus nerve, with its extensive reach, plays a vital role in maintaining homeostasis and regulating various bodily functions. It acts as a communication pathway between the brain and numerous organs, including the heart, lungs, stomach, and intestines. This intricate network of connections allows for efficient coordination and control of essential physiological processes.
As part of the autonomic nervous system, the vagus nerve is responsible for regulating the parasympathetic functions in the body. The parasympathetic nervous system is often referred to as the “rest and digest” system, as it promotes relaxation and recovery. The vagus nerve plays a crucial role in this system by modulating various bodily functions to ensure optimal functioning.
The Role and Function of the Vagus Nerve
The vagus nerve’s primary function is to regulate and maintain the balance of the parasympathetic nervous system. It accomplishes this by sending signals to the organs it innervates, instructing them to slow down and conserve energy. For example, the vagus nerve reduces heart rate, allowing the body to rest and recover.
Furthermore, the vagus nerve stimulates the release of acetylcholine, a neurotransmitter that promotes digestion and increases gastrointestinal motility. This ensures that food is efficiently broken down and absorbed, facilitating the absorption of essential nutrients and promoting overall digestive health.
In addition to its role in the parasympathetic nervous system, the vagus nerve also plays a crucial role in regulating inflammation in the body. It has been found to have anti-inflammatory effects, helping to reduce the body’s immune response and prevent excessive inflammation. This function of the vagus nerve is particularly important in maintaining overall immune system balance and preventing chronic inflammation.
The Difference Between Left and Right Vagus Nerves
While both the left and right branches of the vagus nerve contribute to autonomic control, they have slightly different functions and areas of influence. The left vagus nerve primarily affects the heart, stomach, and other thoracic and upper abdominal organs. It plays a significant role in regulating heart rate, ensuring proper cardiac function, and promoting efficient digestion in the upper gastrointestinal tract.
On the other hand, the right vagus nerve predominantly influences the lower abdominal organs, such as the intestines and bladder. It helps regulate bowel movements, urinary function, and other processes related to the lower gastrointestinal tract. The right vagus nerve’s role in these areas is crucial for maintaining proper digestive and excretory functions.
Overall, the vagus nerve, with its extensive reach and intricate connections, is a vital component of the human body’s regulatory system. Its role in maintaining homeostasis, regulating the parasympathetic nervous system, and modulating inflammation highlights its importance in overall health and well-being.
Identifying Left Vagus Nerve Disorders
Left vagus nerve disorders can manifest in various ways, impacting the affected individual’s daily life and overall well-being.
The left vagus nerve, also known as the cranial nerve X, is one of the main components of the autonomic nervous system. It is responsible for regulating various bodily functions, including heart rate, digestion, and swallowing. When this nerve is disrupted or damaged, it can lead to a range of disorders that affect these functions.
Common Disorders Associated with the Left Vagus Nerve
Disorders related to the left vagus nerve can include conditions like gastroparesis, which is characterized by delayed stomach emptying. This disorder can cause symptoms such as bloating, nausea, vomiting, and a feeling of fullness even after eating small amounts of food.
Atrial fibrillation, another disorder associated with the left vagus nerve, is an irregular heart rhythm that can lead to palpitations, chest pain, and shortness of breath. This condition can significantly impact a person’s quality of life and may require medical intervention to manage the symptoms and reduce the risk of complications.
Additionally, conditions such as functional dyspepsia and gastroesophageal reflux disease (GERD) can also be linked to left vagus nerve dysfunction. Functional dyspepsia is a chronic disorder that affects the upper digestive tract, causing symptoms like stomach pain, bloating, and early satiety. GERD, on the other hand, is a condition where stomach acid flows back into the esophagus, leading to heartburn, regurgitation, and difficulty swallowing.
Recognizing the Symptoms of Left Vagus Nerve Disorders
The symptoms of left vagus nerve disorders can be diverse, and their severity may vary. Patients may experience symptoms such as heart palpitations, which can be described as a racing or irregular heartbeat. Chest pain, often described as a sharp or squeezing sensation, can also be a common symptom.
Difficulty swallowing, known as dysphagia, can occur when the left vagus nerve is affected. This can lead to a sensation of food getting stuck in the throat or chest, making it challenging to eat and drink comfortably. Nausea and vomiting may also be present, causing further discomfort and impacting a person’s ability to maintain proper nutrition.
In addition to gastrointestinal symptoms, left vagus nerve disorders can also manifest as symptoms related to cardiac arrhythmias. Dizziness, lightheadedness, and a feeling of faintness can occur due to the irregular heart rhythm caused by the dysfunction of the left vagus nerve. Shortness of breath, especially during physical exertion, may also be experienced.
It is important to note that the symptoms mentioned above are not exclusive to left vagus nerve disorders and can be caused by various other conditions. Therefore, it is crucial to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
The Causes of Left Vagus Nerve Disorders
Understanding the causes of left vagus nerve disorders is essential in developing effective treatment strategies and preventing further complications. The left vagus nerve, also known as the cranial nerve X, plays a crucial role in regulating various bodily functions, including heart rate, digestion, and respiratory function. When this nerve is affected by disorders, it can lead to a wide range of symptoms and health issues.
Genetic Factors Influencing Left Vagus Nerve Disorders
Studies have demonstrated a potential genetic component in the development of left vagus nerve disorders. Certain genetic variations and mutations may predispose individuals to the malfunctioning of the left vagus nerve, leading to the manifestation of related disorders. Researchers have identified specific genes that may be involved in the regulation and functioning of the left vagus nerve. Understanding these genetic factors can provide valuable insights into the underlying mechanisms of left vagus nerve disorders and potentially lead to targeted treatments.
In addition to genetic factors, other biological factors can influence the development of left vagus nerve disorders. For example, abnormalities in the structure or function of the vagus nerve itself can contribute to its dysfunction. These abnormalities may be present from birth or develop later in life due to various factors, such as trauma or inflammation.
Environmental Factors Contributing to Left Vagus Nerve Disorders
Environmental factors can also contribute to left vagus nerve disorders. Chronic stress, exposure to certain toxins, and a sedentary lifestyle have been associated with an increased risk of developing left vagus nerve-related conditions. Chronic stress can lead to dysregulation of the autonomic nervous system, including the left vagus nerve, causing it to become overactive or underactive. This imbalance can disrupt the normal functioning of the left vagus nerve and contribute to the development of disorders.
Exposure to certain toxins, such as heavy metals or pesticides, can also affect the health of the left vagus nerve. These toxins can directly damage the nerve or interfere with its signaling pathways, leading to dysfunction. Additionally, a sedentary lifestyle characterized by a lack of physical activity can negatively impact the nervous system’s functioning, including the left vagus nerve. Regular exercise and movement are essential for maintaining optimal nerve health and function.
Furthermore, certain medical conditions, such as diabetes or autoimmune disorders, can affect the left vagus nerve. These conditions can cause inflammation or damage to the nerve, leading to its dysfunction. Managing these underlying medical conditions is crucial in preventing or managing left vagus nerve disorders.
In conclusion, the causes of left vagus nerve disorders are multifactorial, involving a combination of genetic, biological, and environmental factors. Understanding these causes is vital for developing effective treatment strategies and preventive measures. By addressing the underlying causes, healthcare professionals can improve the management and outcomes of left vagus nerve disorders, ultimately enhancing the quality of life for affected individuals.
Diagnosing Left Vagus Nerve Disorders
Accurate diagnosis is crucial in managing and treating left vagus nerve disorders effectively. Physicians employ various approaches to diagnose such conditions.
Left vagus nerve disorders can manifest in a variety of ways, including difficulty swallowing, voice changes, and heart rhythm abnormalities. To determine the underlying cause of these symptoms, healthcare professionals utilize a combination of medical history reviews, physical examinations, and diagnostic tests.
Medical History and Physical Examination
A comprehensive medical history review and physical examination play a vital role in diagnosing left vagus nerve disorders. During the medical history review, healthcare professionals carefully assess the patient’s symptoms, medical background, and any previous diagnoses or treatments. This information helps to identify potential causes and narrow down the diagnostic possibilities.
Following the medical history review, a thorough physical examination is conducted. The healthcare professional will examine the patient’s head and neck region, paying close attention to any abnormalities or tenderness. They may also evaluate the patient’s cranial nerve function, including the left vagus nerve, by checking for specific reflexes and responses.
By combining the information gathered from the medical history review and physical examination, healthcare professionals can begin to form a preliminary diagnosis and determine the appropriate next steps for further evaluation.
Diagnostic Tests for Left Vagus Nerve Disorders
In addition to the medical history and physical examination, diagnostic tests are often conducted to confirm the presence of left vagus nerve disorders. These tests provide objective data and help healthcare professionals gain a more comprehensive understanding of the patient’s condition.
One common diagnostic test used to assess left vagus nerve function is an electrocardiogram (ECG). This non-invasive test records the electrical activity of the heart and can detect any abnormalities in heart rhythm that may be caused by vagus nerve dysfunction.
Another diagnostic test frequently employed is esophageal manometry. This procedure involves inserting a thin tube into the esophagus to measure the strength and coordination of the muscles involved in swallowing. By evaluating the function of the esophagus, healthcare professionals can identify any abnormalities that may be attributed to left vagus nerve disorders.
In some cases, imaging modalities, such as ultrasound or magnetic resonance imaging (MRI), may be utilized to visualize the organs affected by vagus nerve dysfunction. These imaging tests provide detailed images of the structures surrounding the left vagus nerve, allowing healthcare professionals to identify any anatomical abnormalities or areas of compression.
By combining the results of these diagnostic tests with the information gathered from the medical history review and physical examination, healthcare professionals can make a more accurate diagnosis of left vagus nerve disorders. This enables them to develop an individualized treatment plan tailored to the patient’s specific needs.
Treatment Options for Left Vagus Nerve Disorders
Effective treatment strategies can help alleviate the symptoms and manage left vagus nerve disorders, improving the patient’s quality of life.
Medications and Therapies for Left Vagus Nerve Disorders
In mild to moderate cases, medications may be prescribed to regulate heart rate, alleviate gastrointestinal symptoms, or manage pain associated with left vagus nerve disorders. Additionally, complementary therapies such as acupuncture, meditation, and deep breathing exercises may provide symptom relief and improve overall well-being.
Surgical Interventions for Severe Cases
In severe cases where conservative treatments fail to relieve symptoms or when complications arise, surgical interventions may be considered. Procedures such as vagotomy, which involve cutting or removing parts of the vagus nerve, are sometimes performed to alleviate the severity of symptoms in specific conditions.
In conclusion, understanding left vagus nerve disorders, their causes, symptoms, and available treatment options is pivotal in providing necessary care and support to individuals affected by these conditions. By fostering a comprehensive understanding of the left vagus nerve’s role and functioning, healthcare professionals can navigate the complexities of diagnosing and managing such disorders effectively, ultimately enhancing patients’ overall well-being.