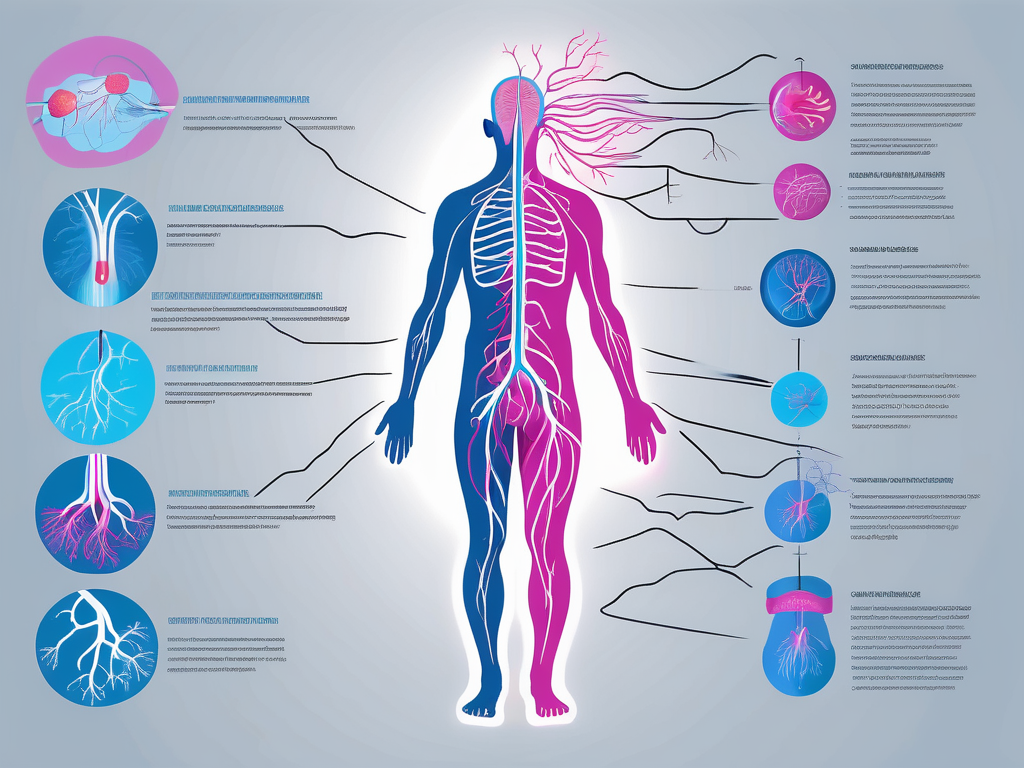
In order to understand extracaraniel vagus nerve disorders, it is important to have a clear knowledge of the vagus nerve itself. The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system. It originates from the brainstem and extends throughout the body, innervating various organs and controlling a wide range of bodily functions.
What is the Vagus Nerve?
The vagus nerve, or cranial nerve X, is the longest and most complex of the cranial nerves. It plays a vital role in regulating numerous bodily processes, including heart rate, digestion, breathing, and even mood. The vagus nerve consists of both motor and sensory fibers, making it a mixed nerve that enables the bidirectional flow of information between the brain and the body.
Role of the Vagus Nerve in the Body
The vagus nerve is responsible for transmitting signals between the brain and various organs, contributing to the regulation of bodily functions both consciously and unconsciously. It helps control heart rate, blood pressure, respiratory rate, and gastrointestinal motility. Additionally, the vagus nerve is involved in the release of neurotransmitters and plays a crucial role in the “rest and digest” response, promoting relaxation and supporting digestion.
When it comes to heart rate regulation, the vagus nerve acts as a brake. It helps to slow down the heart rate when it becomes too fast, ensuring that the heart beats at a steady and controlled pace. This mechanism is particularly important during moments of stress or intense physical activity, as it prevents the heart from overworking and helps maintain cardiovascular health.
In terms of digestion, the vagus nerve plays a significant role in coordinating the movement of food through the gastrointestinal tract. It stimulates the release of digestive enzymes and increases blood flow to the stomach and intestines, optimizing the absorption of nutrients and promoting healthy digestion. Dysfunction of the vagus nerve can lead to gastrointestinal issues such as gastroparesis, a condition characterized by delayed stomach emptying.
Furthermore, the vagus nerve has been linked to mood regulation and mental health. It is involved in the release of neurotransmitters such as serotonin and dopamine, which are known to play a role in mood regulation. Stimulation of the vagus nerve through techniques like vagus nerve stimulation (VNS) has shown promising results in the treatment of depression and other mood disorders.
Anatomy of the Vagus Nerve
The vagus nerve consists of multiple branches that are distributed throughout the body. It originates in the medulla oblongata, the lower part of the brainstem. From there, it extends down through the neck and branches out to innervate various organs and structures, including the heart, lungs, liver, spleen, stomach, and intestines. The vagus nerve is composed of both motor fibers, which control muscle movements, and sensory fibers, which transmit information from the organs back to the brain.
One of the major branches of the vagus nerve is the recurrent laryngeal nerve, which plays a crucial role in vocal cord function. It innervates the muscles of the larynx, allowing for precise control of voice production and speech. Dysfunction of the recurrent laryngeal nerve can lead to vocal cord paralysis, affecting a person’s ability to speak and causing voice changes.
Another important branch of the vagus nerve is the auricular branch, which innervates the external ear. This branch is involved in transmitting sensory information from the ear to the brain, allowing us to hear and process sounds. It also plays a role in the regulation of blood pressure and heart rate through its connection to the cardiovascular system.
The vagus nerve’s extensive distribution throughout the body highlights its significance in maintaining overall health and well-being. Its intricate network of fibers enables efficient communication between the brain and various organs, ensuring the proper functioning of vital bodily processes.
Understanding Extracaraniel Vagus Nerve Disorders
Extracaraniel vagus nerve disorders refer to conditions that affect the vagus nerve outside of the skull, beyond the point where it exits the brainstem. These disorders can have a significant impact on the functioning of the nerve and can lead to a wide range of symptoms and complications.
The vagus nerve, also known as the tenth cranial nerve, is one of the longest and most important nerves in the body. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and respiratory function. When the vagus nerve is affected by extracaraniel disorders, it can disrupt these essential functions and cause significant discomfort and impairment.
Defining Extracaraniel Vagus Nerve Disorders
Extracaraniel vagus nerve disorders encompass a diverse group of conditions that can affect different parts of the nerve or its surrounding structures. These disorders may arise due to various causes, such as injury, compression, inflammation, or underlying health conditions.
One common cause of extracaraniel vagus nerve disorders is trauma or injury to the neck or chest area. For example, a car accident or a sports-related injury can result in damage to the nerve, leading to dysfunction. In some cases, tumors or growths near the vagus nerve can also cause compression and affect its normal functioning.
Inflammation is another factor that can contribute to extracaraniel vagus nerve disorders. Conditions like autoimmune diseases, viral infections, or certain medications can trigger an immune response that mistakenly attacks the nerve, causing inflammation and subsequent dysfunction.
Common Types of Extracaraniel Vagus Nerve Disorders
Extracaraniel vagus nerve disorders can manifest in different ways and present with a variety of symptoms. Some of the common types include vagal neuropathy, vagal paraganglioma, vagal schwannoma, and vagal neuralgia. Each of these conditions has its unique characteristics and requires tailored treatment approaches.
Vagal neuropathy refers to damage or dysfunction of the vagus nerve, leading to impaired communication between the brain and various organs. This can result in symptoms such as difficulty swallowing, hoarseness, and problems with digestion.
Vagal paraganglioma and vagal schwannoma are both types of tumors that can develop near the vagus nerve. These tumors can cause compression and disrupt the normal functioning of the nerve. Symptoms may include voice changes, difficulty breathing, and swallowing difficulties.
Vagal neuralgia is a condition characterized by severe, stabbing pain along the distribution of the vagus nerve. This pain can be triggered by certain activities, such as swallowing or speaking, and can significantly impact a person’s quality of life.
Diagnosing and treating extracaraniel vagus nerve disorders requires a comprehensive evaluation by a healthcare professional. Depending on the specific condition, treatment options may include medication, physical therapy, or surgical interventions.
It is important for individuals experiencing symptoms related to extracaraniel vagus nerve disorders to seek medical attention promptly. Early diagnosis and intervention can help manage symptoms, improve quality of life, and prevent potential complications.
Causes of Extracaraniel Vagus Nerve Disorders
Several factors can contribute to the development of extracaraniel vagus nerve disorders. It is essential to identify and understand these underlying causes to provide effective treatment and management strategies for affected individuals.
Understanding the causes of extracaraniel vagus nerve disorders is crucial in order to develop targeted interventions and improve patient outcomes. Let’s explore some of the key factors that can contribute to the development of these disorders.
Genetic Factors
Genetic mutations or abnormalities can increase the susceptibility to vagus nerve disorders. Some individuals may inherit certain genetic variations that affect the development, structure, or functioning of the nerve, leading to an increased risk of disorders.
Research has shown that specific gene mutations can disrupt the normal growth and development of the vagus nerve. These genetic variations can alter the nerve’s structure or impair its ability to transmit signals effectively. Understanding the genetic basis of these disorders can help in identifying individuals who may be at higher risk and developing targeted therapies.
Environmental Triggers
Exposure to certain environmental factors can also play a role in the development of vagus nerve disorders. These triggers may include physical trauma, such as accidents or injuries, as well as environmental toxins or infections that affect the nerve’s integrity and function.
Physical trauma, such as a car accident or a fall, can directly damage the vagus nerve or the surrounding structures, leading to the development of disorders. Additionally, exposure to environmental toxins, such as certain chemicals or pollutants, can have a detrimental effect on the nerve’s health. Infections, such as viral or bacterial infections, can also cause inflammation and damage to the vagus nerve.
Underlying Health Conditions
Various underlying health conditions, such as autoimmune disorders, tumors, or systemic illnesses, can impact the vagus nerve and contribute to the development of disorders. These conditions may disrupt the normal function of the nerve or cause compression or inflammation in its vicinity.
Autoimmune disorders, such as multiple sclerosis or Guillain-Barré syndrome, can lead to the body’s immune system attacking the vagus nerve, resulting in dysfunction. Tumors or growths in the vicinity of the nerve can exert pressure on it, interfering with its normal functioning. Systemic illnesses, such as diabetes or cardiovascular diseases, can also affect the vagus nerve due to their impact on overall health and nerve function.
Identifying and managing these underlying health conditions is crucial in the treatment of vagus nerve disorders. By addressing the root cause, healthcare professionals can develop comprehensive treatment plans that target both the underlying condition and the associated nerve dysfunction.
Recognizing the Symptoms of Extracaraniel Vagus Nerve Disorders
Extracaraniel vagus nerve disorders can present with a wide range of symptoms, which can vary depending on the specific disorder and the structures affected. Recognizing these symptoms is crucial for timely diagnosis and appropriate management.
The vagus nerve, also known as the tenth cranial nerve, plays a vital role in regulating various bodily functions. It is responsible for controlling the muscles of the throat, voice box, heart, and digestive system. When this nerve is affected by a disorder, it can lead to a variety of physical, emotional, and psychological symptoms.
Physical Symptoms
Physical symptoms of vagus nerve disorders may include difficulty swallowing, voice hoarseness, abnormal heart rate or rhythm, gastrointestinal problems such as nausea, vomiting, or bloating, and respiratory difficulties. These symptoms can be distressing and impact an individual’s ability to carry out daily activities.
Difficulty swallowing, known as dysphagia, can make it challenging to eat and drink. It may feel as though food is getting stuck in the throat or chest, causing discomfort and a risk of choking. Voice hoarseness, on the other hand, can affect the quality of speech and make communication difficult.
Abnormal heart rate or rhythm, also known as arrhythmia, can lead to palpitations, dizziness, and shortness of breath. These symptoms can be alarming and may require medical intervention. Gastrointestinal problems such as nausea, vomiting, and bloating can cause discomfort and affect an individual’s appetite and digestion.
Respiratory difficulties, including shortness of breath and difficulty breathing, can be particularly concerning. These symptoms may indicate a more severe vagus nerve disorder and require immediate medical attention. Changes in blood pressure or sweating patterns may also be observed, further highlighting the impact of vagus nerve dysfunction on the body.
Emotional and Psychological Symptoms
Vagus nerve disorders can also impact an individual’s emotional and psychological well-being. Symptoms such as anxiety, depression, mood swings, and sleep disturbances may be observed. These symptoms can significantly affect an individual’s quality of life and require appropriate psychological support and management.
Anxiety and depression can be debilitating, making it challenging to cope with everyday life. Mood swings, characterized by sudden changes in emotions, can further contribute to emotional instability. Sleep disturbances, such as insomnia or excessive sleepiness, can disrupt the sleep-wake cycle and lead to fatigue and daytime drowsiness.
It is important to note that the relationship between vagus nerve disorders and emotional and psychological symptoms is complex. While the exact mechanisms are not fully understood, it is believed that the vagus nerve plays a role in regulating mood and emotions. Therefore, when this nerve is affected, it can lead to imbalances in neurotransmitters and contribute to the development of mood disorders.
Managing the emotional and psychological symptoms associated with vagus nerve disorders often requires a multidisciplinary approach. This may involve a combination of medication, therapy, lifestyle modifications, and stress management techniques. It is essential for individuals experiencing these symptoms to seek professional help and support.
Diagnostic Procedures for Extracaraniel Vagus Nerve Disorders
Accurate diagnosis of extracaraniel vagus nerve disorders is essential to guide appropriate treatment interventions. Several diagnostic procedures are available to assess the function and integrity of the vagus nerve.
Medical History and Physical Examination
A comprehensive medical history, including any relevant symptoms or prior medical conditions, is essential in the diagnostic process. Additionally, a thorough physical examination by a healthcare professional can provide valuable insights into the potential involvement of the vagus nerve.
Imaging Tests
Imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be employed to visualize the vagus nerve and surrounding structures. These tests can help identify any structural abnormalities, tumors, or areas of compression or inflammation that may be contributing to the disorder.
Neurological Examinations
Neurological examinations, including assessments of reflexes, muscle strength, and sensory perception, can help gauge the functioning of the vagus nerve. These tests, conducted by specialized healthcare professionals, provide valuable information about the nerve’s integrity and potential areas of dysfunction.
Treatment Options for Extracaraniel Vagus Nerve Disorders
The treatment strategies for extracaraniel vagus nerve disorders depend on the underlying cause, severity of symptoms, and individual patient factors. It is important to consider a multidisciplinary approach to address both the physical and psychological aspects of these disorders.
Treatment options may include medications to manage specific symptoms, such as pain relievers or anti-inflammatory drugs. In some cases, surgical interventions may be necessary to address structural abnormalities or remove tumors that are affecting the vagus nerve. Additionally, physical therapy, speech therapy, and other supportive interventions may be employed to help manage symptoms and improve overall functioning.
In conclusion, understanding the causes, symptoms, and treatment options for extracaraniel vagus nerve disorders is crucial for healthcare professionals and patients alike. By recognizing the importance of the vagus nerve and its role in regulating various bodily functions, appropriate care and support can be provided to individuals experiencing these disorders. Continued research and advancements in diagnosis and treatment are essential to improve outcomes for those affected by extracaraniel vagus nerve disorders.