The human body is a complex network of systems and organs, all working together to maintain overall health. Among these vital components, the vagus nerve and the hiatal hernia play crucial roles, affecting various bodily functions. Understanding the relationship between vagus nerve disorders and hiatal hernia is essential in comprehending their impact on individuals’ well-being.
An Overview of Vagus Nerve Disorders
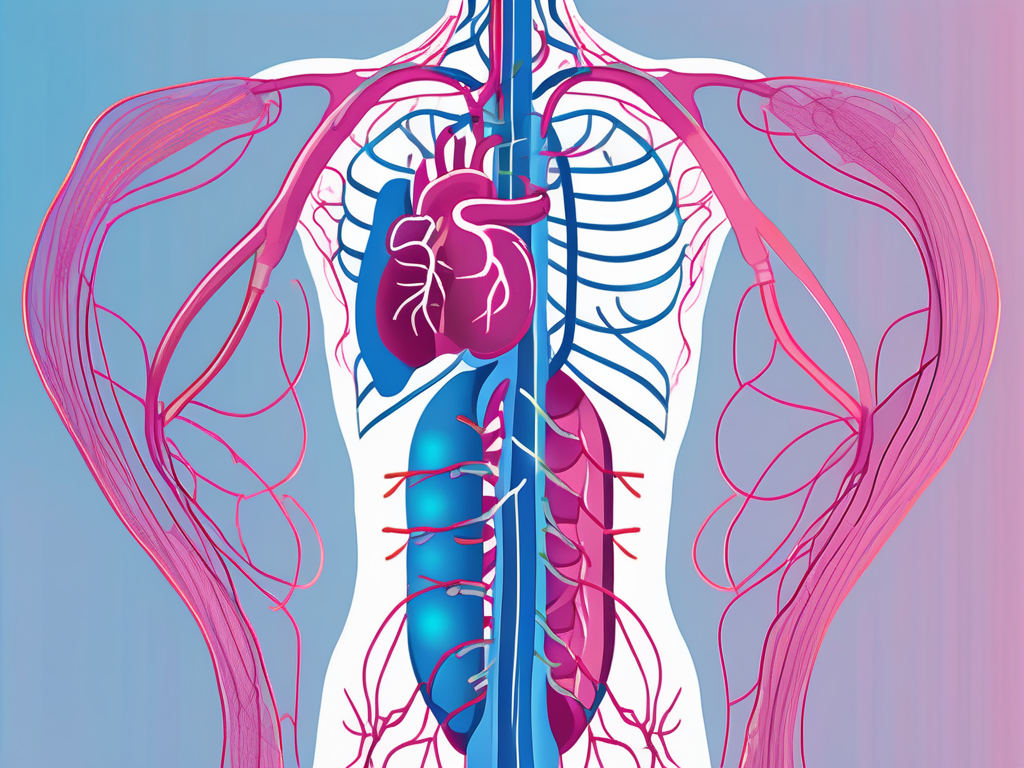
The vagus nerve, also known as the cranial nerve X, is the longest and most intricate cranial nerve in the human body. It originates in the brain, extending down through the chest and abdomen. This crucial nerve is responsible for controlling functions of the parasympathetic nervous system, overseeing activities such as digestion, heart rate, and respiratory function.
The vagus nerve is a complex network of fibers that branches out to various organs and tissues in the body. It plays a vital role in maintaining homeostasis and ensuring the proper functioning of multiple bodily systems. However, like any other part of the body, the vagus nerve can be susceptible to disorders that can disrupt its normal functioning.
Defining Vagus Nerve Disorders
Vagus nerve disorders encompass a range of conditions that affect the proper functioning of the vagus nerve. These disorders can stem from various causes, including injury, infection, or underlying medical conditions. Issues with the vagus nerve can disrupt the intricate balance of bodily functions it governs, leading to a host of symptoms and complications.
One common vagus nerve disorder is called vagus nerve neuropathy, which refers to damage or dysfunction of the nerve. This can occur due to trauma, such as a car accident or a surgical procedure, or as a result of certain medical conditions like diabetes or autoimmune disorders. Another condition, known as vagus nerve compression, happens when the nerve gets compressed or squeezed by nearby structures, leading to impaired function.
Symptoms and Diagnosis of Vagus Nerve Disorders
Recognizing the symptoms of vagus nerve disorders is crucial for timely diagnosis and treatment. Symptoms can vary widely and may include digestive problems such as nausea, vomiting, or difficulty swallowing, as well as heart rate irregularities and breathing difficulties. Some individuals may also experience voice changes, hoarseness, or a persistent cough.
Diagnosing vagus nerve disorders requires a comprehensive approach. Medical professionals will typically begin by conducting a thorough medical history review, looking for any potential risk factors or underlying conditions. A physical examination may also be performed to assess the patient’s overall health and identify any visible signs of vagus nerve dysfunction.
In addition to these initial assessments, specialized tests may be ordered to evaluate the function of the vagus nerve. These tests can include nerve conduction studies, which measure the speed and strength of electrical signals transmitted along the nerve, and imaging studies like magnetic resonance imaging (MRI) or computed tomography (CT) scans to visualize the nerve and surrounding structures.
Treatment Options for Vagus Nerve Disorders
As the understanding of vagus nerve disorders improves, treatment options continue to evolve. The choice of treatment depends on the specific disorder and its severity, as well as the individual’s overall health and preferences.
In cases where vagus nerve disorders are caused by underlying medical conditions, treating the primary condition may help alleviate symptoms and restore normal vagus nerve function. For example, managing diabetes through medication and lifestyle changes can help prevent further nerve damage and improve overall nerve health.
Medications may also be prescribed to manage symptoms associated with vagus nerve disorders. These can include medications to control heart rate, reduce nausea and vomiting, or alleviate pain. Physical therapy may be recommended to improve muscle strength and coordination, especially in cases where vagus nerve dysfunction affects swallowing or voice production.
In some instances, surgical interventions may be necessary to repair or bypass damaged sections of the vagus nerve. These procedures aim to restore normal nerve function and alleviate symptoms. However, surgery is typically considered a last resort when other treatment options have been exhausted or when the condition is severe and significantly impacting the individual’s quality of life.
Alternative therapies, such as acupuncture or biofeedback, may also be explored as adjunctive treatments for vagus nerve disorders. These approaches focus on stimulating the body’s natural healing mechanisms and promoting relaxation and stress reduction, which can have a positive impact on vagus nerve function.
Overall, the management of vagus nerve disorders requires a multidisciplinary approach, involving collaboration between neurologists, gastroenterologists, cardiologists, and other healthcare professionals. By addressing the underlying causes and symptoms of vagus nerve disorders, individuals can experience improved quality of life and better overall health.
Comprehensive Look at Hiatal Hernia
A hiatal hernia occurs when a portion of the stomach pushes through the diaphragm, the muscle that separates the chest cavity from the abdomen. It is estimated that up to 60% of individuals over the age of 50 have some degree of hiatal hernia, although many remain asymptomatic.
Hiatal hernias are classified into two types: sliding hiatal hernia and paraesophageal hiatal hernia. In a sliding hiatal hernia, the stomach and the junction between the stomach and the esophagus slide up into the chest through the hiatus. This is the most common type of hiatal hernia. On the other hand, a paraesophageal hiatal hernia occurs when a portion of the stomach pushes through the hiatus and lies beside the esophagus. This type of hernia is less common but can be more serious as it may lead to complications such as gastric volvulus or strangulation.
What is a Hiatal Hernia?
A hiatal hernia occurs when the upper part of the stomach protrudes into the chest cavity through the hiatus, an opening in the diaphragm. This displacement can result in the stomach’s acid and digestive enzymes leaking into the esophagus, leading to discomfort and various symptoms.
The exact cause of hiatal hernia is not always clear, but there are several factors that can contribute to its development. These include weakened muscles in the diaphragm, increased pressure in the abdomen due to obesity or pregnancy, aging, and certain activities that put strain on the abdominal muscles like heavy lifting or persistent coughing.
Identifying Symptoms of Hiatal Hernia
The symptoms of hiatal hernia can vary widely, with many individuals experiencing no noticeable signs. However, when symptoms do occur, they commonly include heartburn, regurgitation of stomach acid, chest pain, difficulty swallowing, and a feeling of fullness after eating. These symptoms can significantly impact individuals’ quality of life, leading to discomfort and decreased overall well-being.
In addition to these common symptoms, some individuals may also experience respiratory problems such as coughing, wheezing, or shortness of breath. This occurs when the herniated stomach presses against the diaphragm, causing irritation and affecting lung function. It is important to note that these respiratory symptoms can sometimes be mistaken for other conditions, so a proper diagnosis is crucial.
Available Treatments for Hiatal Hernia
The treatment options for hiatal hernia depend on the severity of symptoms and complications. Mild cases may be managed through lifestyle changes, such as maintaining a healthy weight, avoiding trigger foods, and practicing good posture. Elevating the head of the bed while sleeping can also help reduce symptoms by preventing stomach acid from flowing back into the esophagus.
In more severe cases, medications to reduce stomach acid production, such as proton pump inhibitors or H2 blockers, may be prescribed. These medications can provide relief by decreasing the amount of acid in the stomach and reducing the risk of acid reflux. However, it is important to use them under medical supervision and for a limited duration, as long-term use may have potential side effects.
In cases where lifestyle changes and medications are not effective, surgical intervention may be necessary. The most common surgical procedure for hiatal hernia is called Nissen fundoplication. This procedure involves wrapping the upper part of the stomach around the lower esophagus to strengthen the lower esophageal sphincter and prevent acid reflux. Other surgical techniques, such as laparoscopic repair or robotic-assisted surgery, may also be used depending on the individual’s specific condition and the surgeon’s expertise.
It is important to consult with a healthcare professional if you suspect you have a hiatal hernia or are experiencing symptoms related to it. They can perform a thorough evaluation, including physical examination and diagnostic tests such as endoscopy or imaging studies, to confirm the diagnosis and recommend the most appropriate treatment plan.
The Connection Between Vagus Nerve Disorders and Hiatal Hernia
Understanding the intricate relationship between vagus nerve disorders and hiatal hernia sheds light on how these conditions can influence each other’s development and progression.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system. It extends from the brainstem to various organs in the body, including the esophagus and the diaphragm. Dysfunction of the vagus nerve can have far-reaching effects on these structures, impacting their normal functioning and potentially leading to the development of hiatal hernia.
How Vagus Nerve Disorders Can Lead to Hiatal Hernia
Vagus nerve disorders can impact the esophagus and the diaphragm, both of which play critical roles in the development and maintenance of hiatal hernia. The esophagus is a muscular tube that connects the throat to the stomach, allowing the passage of food and liquids. The diaphragm, on the other hand, is a dome-shaped muscle that separates the chest cavity from the abdominal cavity.
When the vagus nerve is functioning properly, it helps coordinate the movement of the esophagus and the diaphragm. This coordination ensures that the diaphragm contracts and relaxes appropriately during breathing, while also allowing the esophagus to propel food downward into the stomach. However, when the vagus nerve is disrupted or damaged, this coordinated movement can be compromised.
The weakening of the hiatus, a small opening in the diaphragm through which the esophagus passes, is a key factor in the development of hiatal hernia. The hiatus acts as a barrier, keeping the stomach and its contents below the diaphragm. However, when the vagus nerve is dysfunctional, the coordinated movement of the diaphragm and the esophagus may be disrupted, leading to increased pressure on the hiatus. This increased pressure can cause the hiatus to weaken, allowing a portion of the stomach to protrude into the chest cavity, resulting in a hiatal hernia.
The Role of the Vagus Nerve in Hiatal Hernia
The vagus nerve plays a vital role in ensuring the proper functioning of the lower esophageal sphincter (LES). The LES is a ring of muscle located at the junction between the esophagus and the stomach. Its primary function is to act as a valve, preventing stomach acid from flowing back into the esophagus.
When the vagus nerve is functioning correctly, it helps regulate the tone and contraction of the LES. This regulation ensures that the LES remains closed when it should, preventing the backflow of stomach acid. However, when the vagus nerve is impaired, the LES may not function properly, leading to a condition known as gastroesophageal reflux disease (GERD).
GERD is characterized by the frequent and persistent backflow of stomach acid into the esophagus. The constant exposure of the esophageal lining to stomach acid can cause inflammation, irritation, and damage, contributing to the development or exacerbation of hiatal hernia.
In summary, the intricate relationship between vagus nerve disorders and hiatal hernia highlights the importance of proper vagus nerve function in maintaining the integrity of the esophagus, the diaphragm, and the lower esophageal sphincter. Dysfunction of the vagus nerve can disrupt the coordinated movement of these structures, weaken the hiatus, and compromise the function of the LES, all of which can contribute to the development and progression of hiatal hernia.
The Impact of Co-Existing Vagus Nerve Disorders and Hiatal Hernia
When individuals experience both vagus nerve disorders and hiatal hernia simultaneously, the resulting complications can significantly affect their overall well-being.
Complications Arising from Concurrent Disorders
Co-existing vagus nerve disorders and hiatal hernia can lead to a variety of complications. These may include worsening symptoms of acid reflux and gastroesophageal reflux disease (GERD), difficulty in eating and drinking, inadequate absorption of nutrients, and an increased risk of esophageal ulcers and strictures. Additionally, the associated discomfort and pain can impact individuals’ quality of life and mental health.
Managing Dual Diagnosis: Vagus Nerve Disorders and Hiatal Hernia
Managing the dual diagnosis of vagus nerve disorders and hiatal hernia requires a multidisciplinary approach involving healthcare professionals from various specialties. Treatment strategies may involve a combination of medications to manage symptoms, dietary changes to alleviate acid reflux, physical therapy to promote vagus nerve function, and surgical interventions to repair the hernia and address vagus nerve dysfunction.
Future Research and Developments
Ongoing research and advancements in understanding the link between vagus nerve disorders and hiatal hernia hold promise for improved diagnosis and treatment approaches.
Advances in Understanding the Link
Researchers continue to explore the complex relationship between vagus nerve disorders and hiatal hernia, aiming to uncover additional mechanisms and potential therapeutic targets. Improved understanding of the link between these conditions may lead to enhanced diagnostic tools and more targeted treatment options, ultimately improving the quality of life for those affected.
Potential Breakthroughs in Treatment Options
Advances in medical science and technology offer hope for innovative treatment options. Ongoing research into non-invasive therapies, such as neurostimulation, may provide alternative approaches to managing vagus nerve disorders and hiatal hernia, reducing the need for invasive procedures and alleviating symptoms more effectively.
In conclusion, an in-depth understanding of the interplay between vagus nerve disorders and hiatal hernia is essential in providing comprehensive care and improving individuals’ well-being. By further exploring the connection, identifying symptoms, and developing targeted treatments, healthcare professionals can address these conditions more effectively, offering a brighter future for those affected.