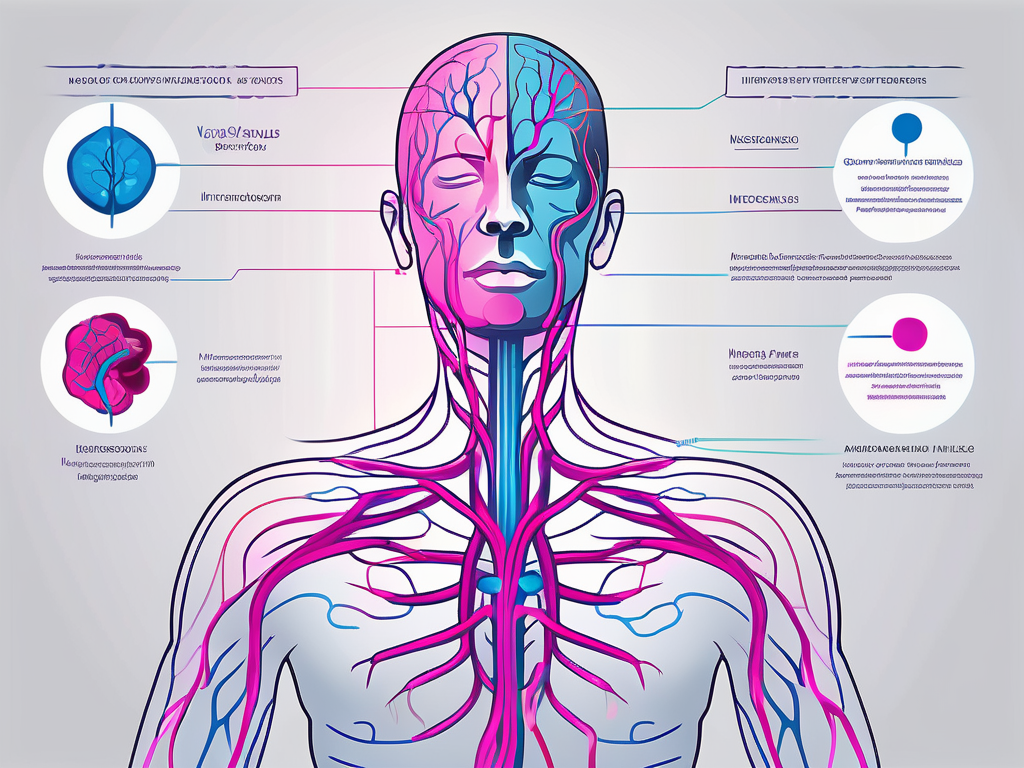
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions. It is a key component of the autonomic nervous system, responsible for controlling involuntary actions such as heart rate, digestion, and respiratory function. However, when this vital nerve is affected by autoimmune disorders, it can lead to significant disruptions in the body’s normal functioning.
What is the Vagus Nerve?
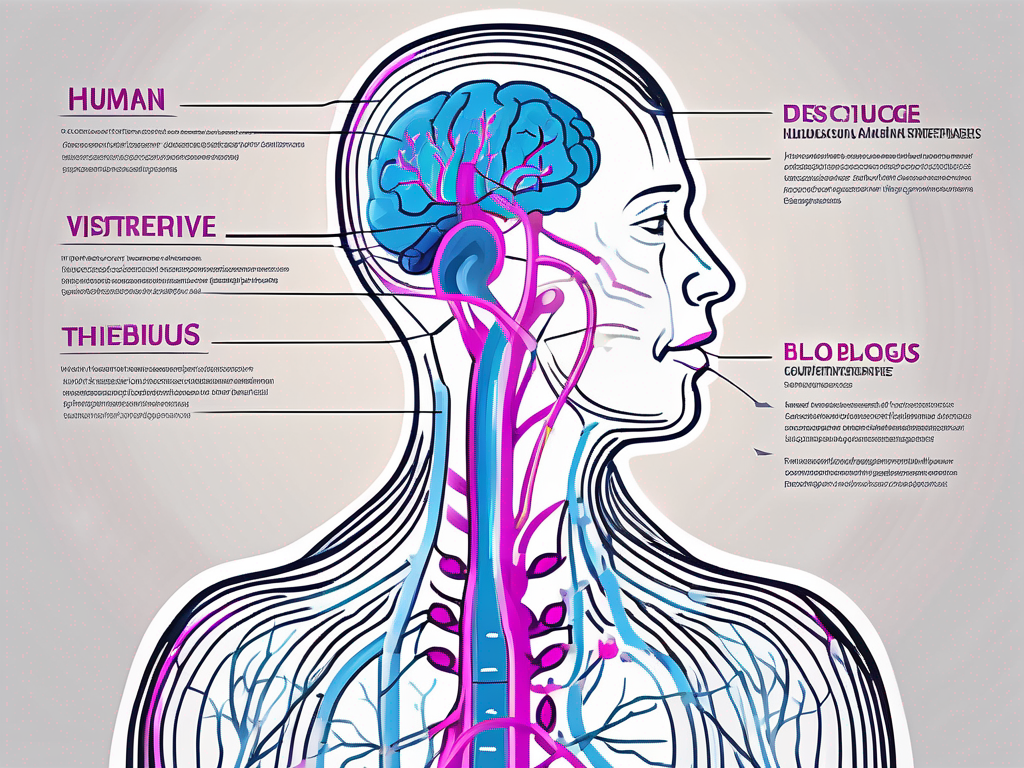
The vagus nerve, scientifically known as the cranial nerve X, is the longest and most complex of the cranial nerves. It originates in the medulla oblongata, located at the base of the brainstem, and extends down through the neck and thorax to the abdomen, innervating various organs along its course. This extensive reach enables it to regulate numerous bodily processes and maintain homeostasis.
The vagus nerve is a fascinating structure that has captivated the attention of researchers and medical professionals for centuries. Its name, “vagus,” is derived from the Latin word for “wandering,” which perfectly describes its meandering path through the body. This wandering nature allows the vagus nerve to establish connections with a wide array of organs and tissues, making it a crucial component of the body’s intricate neural network.
Throughout history, the vagus nerve has been linked to various physiological and psychological phenomena. Ancient Greek physicians recognized its role in controlling the voice and influencing speech, while modern scientists have uncovered its involvement in regulating heart rate, digestion, and even emotional responses. The vagus nerve truly embodies the complexity and interconnectedness of the human body.
The Role and Function of the Vagus Nerve
The vagus nerve plays a critical role in the parasympathetic division of the autonomic nervous system, commonly referred to as the “rest and digest” system. Its primary function is to facilitate communication between the brain and the major organs, including the heart, lungs, stomach, and intestines. Through its branches, the vagus nerve controls heart rate, gastrointestinal motility, respiratory rate, and even modulates immune responses.
One of the most remarkable aspects of the vagus nerve’s function is its ability to sense and respond to changes in the body’s internal environment. It constantly receives feedback from various organs and relays this information to the brain, allowing for real-time adjustments to maintain equilibrium. For example, if the body requires increased blood flow to the digestive system after a meal, the vagus nerve will signal the heart to pump more blood and stimulate the release of digestive enzymes.
Furthermore, the vagus nerve is involved in the regulation of inflammation. It has been shown to exert anti-inflammatory effects by inhibiting the release of pro-inflammatory molecules and promoting the production of anti-inflammatory substances. This mechanism highlights the vagus nerve’s role in maintaining immune balance and preventing excessive immune responses that can lead to chronic inflammation and disease.
The Vagus Nerve and the Autonomic Nervous System
The autonomic nervous system is responsible for regulating physiological processes that occur automatically, without conscious effort. It consists of two divisions: the sympathetic and parasympathetic nervous systems. While the sympathetic division prepares the body for fight-or-flight responses, the parasympathetic division, with the help of the vagus nerve, maintains a state of calm and relaxation by counterbalancing the sympathetic activity.
When the body perceives a threat or stressor, the sympathetic nervous system activates, triggering a cascade of physiological changes designed to prepare the body for action. This includes increased heart rate, heightened alertness, and decreased digestive activity. However, once the threat has passed, the parasympathetic division, led by the vagus nerve, takes over to restore equilibrium and promote recovery.
By influencing the release of neurotransmitters such as acetylcholine, the vagus nerve helps to slow heart rate, improve digestion, promote relaxation, and enhance overall well-being. This intricate interplay between the vagus nerve and the autonomic nervous system ensures optimal functioning of the body’s vital processes.
It is important to note that the vagus nerve’s role extends beyond its involvement in the autonomic nervous system. Recent research has uncovered its potential influence on various mental health conditions, such as depression, anxiety, and even post-traumatic stress disorder. Scientists are actively investigating the therapeutic potential of stimulating the vagus nerve to alleviate symptoms and improve overall mental well-being.
In conclusion, the vagus nerve is a remarkable structure that serves as a vital link between the brain and the body’s major organs. Its extensive reach and intricate functions make it a key player in maintaining homeostasis, regulating physiological processes, and even influencing mental health. The more we uncover about the vagus nerve, the more we realize its significance in our overall well-being.
Defining Autoimmune Disorders
Autoimmune disorders occur when the immune system mistakenly attacks healthy cells and tissues within the body. Normally, the immune system acts as a defense mechanism against foreign invaders, such as bacteria and viruses. However, in the case of autoimmune disorders, the immune system becomes confused and starts targeting its own cells, leading to inflammation and damage.
When the immune system is functioning properly, it is a complex network of cells, tissues, and organs that work together to protect the body from harmful substances. It relies on the ability to distinguish between self and non-self antigens. This self-tolerance is crucial for maintaining a healthy immune response. However, when this self-tolerance breaks down, the immune system can start attacking healthy tissues, giving rise to autoimmune disorders.
Autoimmunity can be triggered by various factors, including genetic predisposition, hormonal imbalances, and environmental triggers. The exact mechanisms behind the development of autoimmunity remain elusive, but researchers have identified several mechanisms that contribute to the breakdown of self-tolerance.
One mechanism involves the production of autoantibodies, which are antibodies that mistakenly target the body’s own tissues. These autoantibodies can bind to specific antigens on healthy cells, leading to inflammation and tissue damage. Another mechanism involves the activation of autoreactive T cells, which are immune cells that mistakenly recognize self-antigens as foreign. These activated T cells can then initiate an immune response against healthy tissues.
Common Types of Autoimmune Disorders
Autoimmune disorders can affect virtually any organ or system in the body. Some of the most common autoimmune disorders include:
- Rheumatoid arthritis: This autoimmune disorder primarily affects the joints, causing pain, stiffness, and swelling. It can also affect other organs, such as the heart and lungs.
- Lupus: Lupus is a systemic autoimmune disorder that can affect multiple organs, including the skin, joints, kidneys, and heart. It is characterized by a wide range of symptoms, including fatigue, joint pain, skin rashes, and kidney problems.
- Multiple sclerosis: This autoimmune disorder affects the central nervous system, leading to the destruction of the protective covering of nerve fibers. It can cause a wide range of symptoms, including muscle weakness, coordination problems, and cognitive impairment.
- Type 1 diabetes: Type 1 diabetes is an autoimmune disorder that affects the pancreas, specifically the cells that produce insulin. It results in the inability to regulate blood sugar levels, leading to symptoms such as excessive thirst, frequent urination, and unexplained weight loss.
- Inflammatory bowel disease: This umbrella term encompasses several autoimmune disorders that affect the digestive tract, including Crohn’s disease and ulcerative colitis. These conditions can cause symptoms such as abdominal pain, diarrhea, and weight loss.
Each autoimmune disorder has its own set of target tissues and symptoms. However, they often share similar underlying pathological processes, such as chronic inflammation, tissue destruction, and altered immune responses. Understanding these commonalities is crucial for gaining insights into the development and treatment of autoimmune disorders.
Researchers are continuously working to unravel the complexities of autoimmune disorders. By studying the underlying mechanisms and identifying potential therapeutic targets, they hope to develop more effective treatments and interventions. Additionally, advancements in personalized medicine and genetic research may lead to improved diagnostic tools and tailored treatment approaches for individuals with autoimmune disorders.
Vagus Nerve Autoimmune Disorders Explained
When autoimmune disorders specifically target the vagus nerve, it can lead to dysregulation of its function and subsequent disruptions in various bodily processes. The effects of vagus nerve autoimmune disorders can be far-reaching, impacting both physical and psychological well-being.
How Autoimmune Disorders Affect the Vagus Nerve
Autoimmune disorders affecting the vagus nerve can lead to inflammation and damage to its branches, affecting the transmission of signals between the brain and the targeted organs. This can result in abnormalities in heart rate, gastrointestinal motility, respiratory function, and immune responses, among others.
Furthermore, inflammation in the vicinity of the vagus nerve can further exacerbate its dysfunction, perpetuating a cycle of immune dysregulation and tissue damage. As a result, individuals with vagus nerve autoimmune disorders may experience a range of symptoms that significantly impact their quality of life.
Identifying Vagus Nerve Autoimmune Disorders
Diagnosing vagus nerve autoimmune disorders can be challenging, as their symptoms often overlap with other medical conditions. A comprehensive evaluation, including a detailed medical history, physical examination, laboratory tests, and imaging studies, is essential for accurate diagnosis.
Diagnostic tests such as electromyography and nerve conduction studies can help assess the integrity and functioning of the vagus nerve. Additionally, specialized tests, such as autonomic function tests and antibody testing, may be employed to evaluate the immune response and identify specific autoimmune markers.
Causes of Vagus Nerve Autoimmune Disorders
Vagus nerve autoimmune disorders can arise from a combination of genetic and environmental factors. While the exact causes remain largely unknown, researchers have made significant strides in understanding the underlying mechanisms contributing to their development.
Genetic Factors and Vagus Nerve Autoimmune Disorders
Genetic predisposition plays a role in the susceptibility to autoimmune disorders, including those affecting the vagus nerve. Certain genetic variations can influence immune system function, increasing the likelihood of developing autoimmune reactions. However, the specific genes involved in vagus nerve autoimmune disorders are still being unraveled through ongoing research.
Family history can also provide valuable insights into the risk of developing autoimmune disorders, as these conditions often cluster within families. Identifying genetic markers associated with vagus nerve autoimmune disorders may aid in early detection and targeted treatments in the future.
Environmental Triggers and Vagus Nerve Autoimmune Disorders
Environmental factors can trigger or exacerbate autoimmune responses in susceptible individuals. These triggers can include infections, exposure to certain chemicals or drugs, hormonal changes, and chronic stress. The interplay between genetic predisposition and environmental triggers is thought to contribute to the development of vagus nerve autoimmune disorders.
Ongoing research aims to unravel the specific environmental factors that interact with the immune system and promote the development of autoimmune reactions. Understanding these triggers may lead to the identification of preventive strategies and more personalized treatment approaches.
Recognizing the Symptoms of Vagus Nerve Autoimmune Disorders
Due to the vast array of bodily functions regulated by the vagus nerve, vagus nerve autoimmune disorders can manifest with a broad spectrum of symptoms. These symptoms can be categorized into physical and psychological manifestations, each affecting individuals differently.
Physical Symptoms and Signs
Physical symptoms of vagus nerve autoimmune disorders can include cardiovascular abnormalities, such as irregular heart rate or blood pressure fluctuations. Gastrointestinal symptoms, such as impaired digestion and motility, may lead to issues like bloating, constipation, or diarrhea. Respiratory difficulties, unexplained fatigue, or unexplained weight fluctuations are also commonly reported.
In addition to these specific symptoms, vagus nerve autoimmune disorders can have a significant impact on overall physical well-being, leading to decreased vitality and an impaired ability to engage in daily activities.
Psychological Symptoms and Signs
Psychological symptoms often accompany physical manifestations in vagus nerve autoimmune disorders. These can include anxiety, depression, cognitive impairments, such as memory and concentration deficits, mood swings, and sleep disturbances. The psychological toll of living with these disorders can be substantial, impacting overall emotional well-being and quality of life.
It is important to note that symptoms may vary from person to person, and some individuals may experience a combination of physical and psychological manifestations. Regular monitoring, support, and appropriate medical interventions can help manage these symptoms and improve overall functioning.
Treatment Approaches for Vagus Nerve Autoimmune Disorders
Given the complex nature of vagus nerve autoimmune disorders, their treatment often requires a multidisciplinary and individualized approach. The primary goals of managing these disorders are to reduce inflammation, modulate immune responses, and alleviate symptoms to improve quality of life.
Treatment options may include pharmacological interventions, such as immunosuppressants or anti-inflammatory medications, to suppress the immune response and reduce inflammation. Additionally, therapies targeting specific symptoms, such as cardiac rhythm management, pain management, and gastrointestinal support, are integral to comprehensive care.
Additional complementary approaches, including stress reduction techniques, dietary modifications, physical therapy, and counseling, can provide valuable adjunctive support in managing the symptoms and promoting overall well-being. It is essential for individuals with vagus nerve autoimmune disorders to work closely with healthcare professionals to develop a comprehensive treatment plan tailored to their individual needs.
Conclusion
Understanding vagus nerve autoimmune disorders is crucial for healthcare professionals and individuals affected by these conditions. By comprehending the role of the vagus nerve in autonomic regulation, the disturbed immune responses in autoimmunity, and the factors contributing to the development of vagus nerve autoimmune disorders, we can strive for earlier detection, improved diagnostics, and more targeted treatment approaches.
Efforts to unravel the complex interplay between genetic and environmental factors, to identify specific genetic markers, and to discover preventive strategies are ongoing. With continued research and collaboration, we can enhance our understanding of vagus nerve autoimmune disorders and develop more effective interventions to alleviate symptom burden and improve the lives of those affected.