Scoliosis and vagus nerve disorders are two distinct medical conditions that may appear unrelated at first glance. However, recent research has shed light on the potential connection between these two seemingly disparate conditions. Understanding this connection is crucial in developing effective treatment strategies and improving patient outcomes. In this article, we will delve into the intricacies of scoliosis and vagus nerve disorders, explore their shared link, and discuss the various treatment options available.
Defining Scoliosis: An Overview
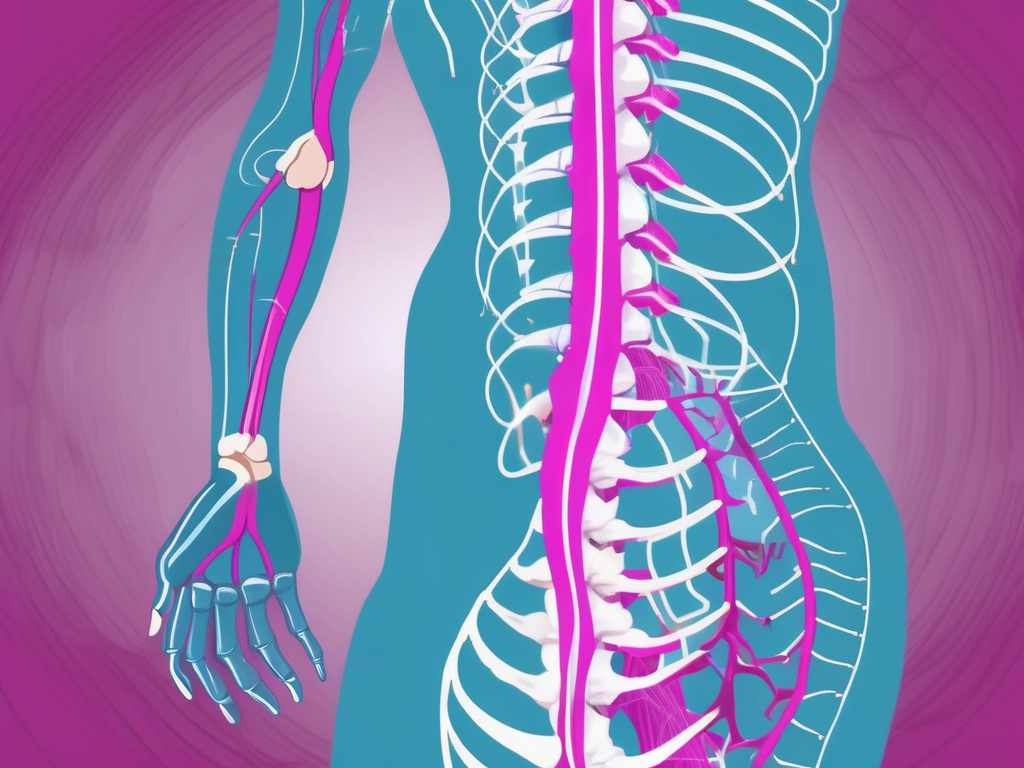
Scoliosis is a musculoskeletal disorder characterized by an abnormal curvature of the spine. Typically, the spine should exhibit a straight alignment when viewed from the back. However, in scoliosis, the spine deviates from its normal vertical position and curves sideways, forming an “S” or a “C” shape. This curvature can affect any part of the spine and may vary in severity.
The Anatomy and Function of the Spine
Before delving deeper into the complexities of scoliosis, it is essential to understand the anatomy and function of the spine. The spine is a crucial component of the musculoskeletal system, providing support, balance, and protection to the delicate spinal cord. Consisting of a series of interconnected bones known as vertebrae, the spine allows for flexibility and facilitates movement while safeguarding the central nervous system.
Each vertebra in the spine is connected by joints and discs that provide cushioning and shock absorption. Moreover, the spine is supported by a network of muscles, ligaments, and tendons, which work in harmony to maintain stability and enable everyday activities.
Furthermore, the spine can be divided into different regions, each with its unique characteristics and functions. The cervical spine, located in the neck region, supports the head and allows for a wide range of motion. The thoracic spine, in the upper back, provides structural support and protects the vital organs in the chest. The lumbar spine, in the lower back, bears the majority of the body’s weight and allows for bending and twisting movements. Finally, the sacral spine, at the base of the spine, connects the spine to the pelvis and plays a role in weight distribution.
The Different Types of Scoliosis
Scoliosis can manifest in various forms, depending on its cause and age of onset. The three primary types of scoliosis are:
- Idiopathic scoliosis: This is the most common form of scoliosis, and its cause remains unknown. It typically develops during adolescence and affects girls more frequently than boys.
- Congenital scoliosis: This form of scoliosis is present at birth and occurs due to abnormalities in the spine’s development during fetal growth. It can be caused by genetic factors or environmental influences.
- Neuromuscular scoliosis: This type of scoliosis arises as a secondary condition to an underlying neuromuscular disorder, such as cerebral palsy or muscular dystrophy. The abnormal muscle control and weakness associated with these conditions can lead to imbalances in the spine.
It is important to note that scoliosis can also be classified based on the age of onset. Infantile scoliosis occurs before the age of 3, juvenile scoliosis develops between the ages of 3 and 10, and adolescent scoliosis occurs between the ages of 10 and 18.
Common Symptoms and Diagnosis of Scoliosis
Individuals with scoliosis may experience various symptoms, ranging from mild to severe, depending on the degree of spinal curvature. Common signs and symptoms include:
- Uneven shoulders or waistline: As the spine curves, it can cause one shoulder or hip to appear higher than the other, resulting in an asymmetrical appearance.
- Asymmetrical posture or leaning to one side: Due to the spinal curvature, individuals with scoliosis may adopt a posture that leans to one side or appears tilted.
- Prominent shoulder blade or rib hump: In some cases, the curvature of the spine can cause the shoulder blade or ribs to protrude more prominently on one side of the body.
- Back pain or discomfort: Scoliosis can lead to back pain, especially in cases where the curvature is severe or progressive.
- Reduced range of motion in the spine: As the spine becomes more curved, it may limit the individual’s ability to move or twist their back comfortably.
- Breathing difficulties in severe cases: In severe cases of scoliosis, where the curvature affects the chest cavity, it can lead to breathing difficulties and reduced lung function.
To diagnose scoliosis, a healthcare professional will conduct a thorough physical examination, including a visual assessment of the back and a series of tests, such as the Adam’s forward bend test. During this test, the individual is asked to bend forward while the healthcare professional observes the alignment of the spine. Any asymmetry or curvature becomes more apparent in this position.
In some cases, further imaging studies, such as X-rays or MRI scans, may be necessary to evaluate the severity and underlying causes of the curvature. These imaging techniques provide detailed images of the spine, allowing healthcare professionals to measure the degree of curvature and assess any structural abnormalities.
Early detection and diagnosis of scoliosis are crucial for effective management and treatment. Regular screenings, especially during adolescence, can help identify scoliosis at an early stage when interventions are most effective. With appropriate medical care and support, individuals with scoliosis can lead fulfilling lives and manage their condition to minimize its impact on their overall well-being.
Unraveling Vagus Nerve Disorders
The vagus nerve, also known as the tenth cranial nerve or the wandering nerve, is a vital component of the autonomic nervous system. It plays a pivotal role in regulating numerous bodily functions, including heart rate, digestion, respiration, and even emotional well-being. Vagus nerve disorders encompass a range of conditions that impact the normal functioning of this crucial nerve.
The vagus nerve originates in the brainstem and extends throughout the body, connecting various organs and tissues. It consists of both sensory and motor fibers, allowing it to transmit signals to and from the brain. This bidirectional communication enables the vagus nerve to influence and regulate diverse physiological processes.
One of the key functions of the vagus nerve is its involvement in the parasympathetic branch of the autonomic nervous system. Activating the vagus nerve helps promote a state of relaxation, reducing heart rate and blood pressure while increasing digestive activity. Additionally, the vagus nerve aids in controlling inflammation, regulating immune responses, and fostering emotional well-being.
Understanding the intricate role of the vagus nerve in the body is essential in comprehending the impact of vagus nerve disorders. These disorders can manifest in a variety of ways, often affecting multiple bodily systems. Some common vagus nerve disorders include:
- Vagal neuropathy: This condition occurs when there is damage or dysfunction of the vagus nerve, leading to impaired function.
- Vasovagal syncope: This disorder involves a sudden drop in heart rate and blood pressure, resulting in fainting or loss of consciousness.
- Gastroparesis: It is a condition characterized by delayed stomach emptying due to inadequate vagal stimulation.
- Vagus nerve stimulation (VNS) complications: In some cases, individuals who have undergone vagus nerve stimulation therapy may experience adverse effects like hoarseness, coughing, or difficulty swallowing.
Identifying vagus nerve disorders can be challenging, as the symptoms may vary depending on the specific condition and organs affected. However, recognizing the signs is crucial for early intervention and appropriate treatment. Some common symptoms of vagus nerve disorders include heart palpitations or irregular heartbeats, digestive disturbances such as nausea, vomiting, or bloating, difficulties swallowing or changes in voice quality, fluctuations in blood pressure, and mood changes or anxiety.
Diagnosing vagus nerve disorders requires a thorough medical evaluation, including a detailed patient history and physical examination. Healthcare professionals may inquire about the onset and duration of symptoms, as well as any potential triggers or exacerbating factors. Additional diagnostic tests, such as electrocardiograms, gastric emptying studies, or nerve conduction studies, may be necessary to assess the functioning of the vagus nerve and eliminate other possible causes for the presenting symptoms.
Expanding our knowledge about vagus nerve disorders is vital for improving diagnosis and treatment options. Ongoing research aims to unravel the underlying mechanisms of these disorders and develop innovative therapies that target the vagus nerve. By understanding the complexities of this remarkable nerve, healthcare professionals can provide better care and support to individuals affected by vagus nerve disorders.
The Intersection of Scoliosis and Vagus Nerve Disorders
While scoliosis and vagus nerve disorders may seem like distinct entities, recent research suggests a potential association between these conditions. The spine and the vagus nerve, although seemingly unrelated, are intricately connected, sharing a complex web of interactions. Understanding the intersection of scoliosis and vagus nerve disorders is crucial in formulating comprehensive treatment approaches.
The Impact of Spinal Health on Nervous System Function
The spine serves as the primary structural support for the body and houses the spinal cord – a vital component of the nervous system. Any abnormalities in spinal alignment, such as those present in scoliosis, can potentially impact nervous system function, including the vagus nerve. Misalignments or compression of nerve structures caused by scoliotic curves could disrupt the communication between the brain and various organ systems, potentially leading to vagus nerve dysfunction.
How Scoliosis Can Affect the Vagus Nerve
The exact mechanisms through which scoliosis affects the vagus nerve are still being elucidated. However, it is theorized that the altered spinal curvature in scoliosis may lead to nerve entrapment or compression, affecting the vagus nerve’s ability to transmit signals effectively. The extent of this impact may depend on factors such as the severity and location of the scoliotic curves.
The Potential Consequences of This Connection
The potential consequences of the connection between scoliosis and vagus nerve disorders are vast and multifaceted. Individuals with scoliosis may experience autonomic dysregulation, including disruptions in heart rate variability, digestive function, and respiratory patterns – all of which are directly influenced by the vagus nerve. Additionally, vagus nerve disorders may exacerbate the already complex physical and psychosocial challenges associated with scoliosis, further compromising quality of life.
Treatment Options for Scoliosis and Vagus Nerve Disorders
The management of scoliosis and vagus nerve disorders requires a comprehensive approach that addresses both the individual conditions and their potential interconnectedness. Several treatment options are available, ranging from non-invasive interventions to surgical procedures.
Non-Surgical Interventions for Scoliosis
In mild to moderate cases of scoliosis, non-surgical interventions may be recommended to manage symptoms, slow down the progression of the curvature, and enhance overall spinal health. These interventions may include:
- Physical therapy exercises, focusing on core strength and posture correction
- Bracing, which involves wearing a spinal brace to help correct the curvature or prevent further progression
- Chiropractic care, with spinal adjustments to improve alignment and reduce muscle imbalances
- Alternative therapies like yoga or Pilates to promote flexibility and movement
Surgical Treatments for Scoliosis
In severe cases of scoliosis or when non-surgical interventions fail to provide adequate relief, surgical procedures may be considered. The goal of scoliosis surgery is to correct the abnormal curvature and stabilize the spine. Surgeons utilize various techniques, such as spinal fusion or instrumentation, to achieve optimal results. However, as with any surgical intervention, scoliosis surgery carries inherent risks and requires careful evaluation and consideration.
Managing Vagus Nerve Disorders: Medication and Therapy
When it comes to treating vagus nerve disorders, the primary focus is on managing symptoms and improving overall vagal tone. Depending on the specific condition, treatment options may include:
- Medications: Certain medications, such as vasopressors or anti-arrhythmics, may be prescribed to regulate heart rate and blood pressure.
- Physical therapy: Targeted exercises can help strengthen the vagus nerve and improve its functioning.
- Biofeedback: This therapy involves training individuals to self-regulate various physiological functions, including heart rate, through conscious control.
- Vagus nerve stimulation (VNS) therapy: In some cases, VNS therapy may be recommended as a way to directly modulate vagus nerve activity and alleviate symptoms.
In conclusion, the connection between scoliosis and vagus nerve disorders represents a complex and often overlooked aspect of these two conditions. By better understanding this connection, healthcare professionals can develop more tailored treatment plans that address the interplay between scoliosis and vagus nerve function. Furthermore, future research endeavors aimed at unraveling the intricacies of this association hold promise in advancing our knowledge and improving patient outcomes.