Vagus nerve disorders can present a wide range of symptoms, making it essential to seek appropriate medical care for accurate diagnosis and targeted treatment. Understanding the role of the vagus nerve in the body, common symptoms of vagus nerve disorders, and potential causes can provide valuable insights into the expertise required by healthcare professionals. In this article, we will explore the different types of doctors who specialize in vagus nerve disorders, diagnostic procedures commonly used, and various treatment options available.
Understanding Vagus Nerve Disorders
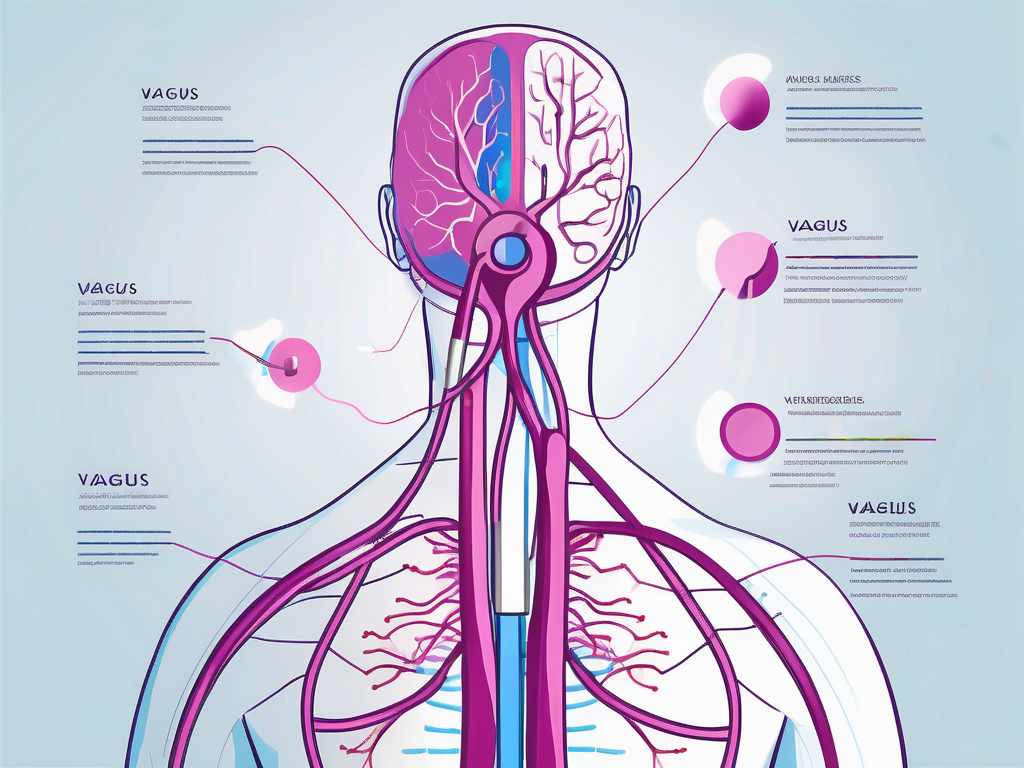
Before delving into the medical specialization involved in the treatment of vagus nerve disorders, it is crucial to have a basic understanding of the condition itself. The vagus nerve, also known as the tenth cranial nerve, plays a critical role in regulating various bodily functions, including heart rate, digestion, and breathing. When the vagus nerve malfunctions, it can lead to a range of symptoms and health issues.
The Role of the Vagus Nerve in the Body
The vagus nerve is the longest cranial nerve and is part of the autonomic nervous system. It originates in the brainstem and extends down to the abdomen, connecting various organs along the way. Its primary function is to facilitate communication between the brain and organs, ensuring their proper functioning.
Some of the key roles of the vagus nerve include regulating heart rate, controlling gastrointestinal movements, stimulating digestive secretions, influencing breathing patterns, and modulating the body’s inflammatory response. Its intricate network of fibers allows it to transmit both sensory and motor signals effectively.
For example, when you eat a meal, the vagus nerve helps stimulate the release of digestive enzymes and promotes the contraction of the muscles in your stomach and intestines, aiding in the digestion process. Additionally, it plays a crucial role in maintaining a steady heart rate by sending signals to the heart to speed up or slow down as needed.
Common Symptoms of Vagus Nerve Disorders
When the vagus nerve experiences dysfunction or damage, it can lead to a variety of symptoms that can be distressing for individuals. These symptoms may include but are not limited to changes in heart rate and blood pressure, gastrointestinal issues such as nausea and vomiting, difficulty swallowing, voice hoarseness, respiratory problems, and abnormal sweating patterns.
For instance, individuals with vagus nerve disorders may notice that their heart rate becomes irregular or that they experience sudden drops in blood pressure, leading to dizziness or fainting. Digestive problems such as frequent nausea or difficulty swallowing can also be indicative of vagus nerve dysfunction. Additionally, some individuals may experience changes in their voice, such as hoarseness, due to the nerve’s role in controlling the muscles involved in speech production.
While vagus nerve disorders can manifest in different ways depending on the specific condition, it is essential to seek medical attention if experiencing any concerning symptoms. Early diagnosis and intervention can significantly improve the management and prognosis of these disorders.
Potential Causes of Vagus Nerve Disorders
Vagus nerve disorders can arise due to various underlying causes, such as trauma or injury to the nerve, infections like Lyme disease or viral infections, autoimmune diseases that affect the nervous system, tumors or growths compressing the nerve, or other systemic conditions affecting nerve function. Identifying the root cause of the disorder is crucial for effective treatment and management.
For example, a person who has been involved in a car accident and experienced trauma to the neck area may develop vagus nerve dysfunction as a result. Infections, such as Lyme disease, can also affect the nerve and lead to symptoms of vagus nerve disorders. Additionally, autoimmune diseases like multiple sclerosis or Guillain-Barré syndrome can cause inflammation and damage to the vagus nerve, resulting in dysfunction.
It is important for healthcare professionals to conduct a thorough evaluation and diagnostic tests to determine the underlying cause of vagus nerve disorders. This information is vital in developing an appropriate treatment plan and addressing the specific needs of each individual.
Different Types of Doctors for Vagus Nerve Disorders
Given the complexity and multisystem involvement of vagus nerve disorders, several medical specialists play a significant role in their diagnosis and treatment. Seeking the right doctor can ensure a comprehensive approach to care and optimize outcomes for those affected.
Neurologists and Vagus Nerve Disorders
Neurologists are physicians who specialize in the diagnosis and treatment of diseases and disorders affecting the nervous system. This includes vagus nerve disorders, as they are primarily concerned with conditions related to the brain, spinal cord, and peripheral nerves. Neurologists often conduct detailed neurological examinations, order and interpret imaging studies, and recommend appropriate treatment strategies based on the individual’s specific condition.
When it comes to vagus nerve disorders, neurologists are at the forefront of understanding the intricate connections between the vagus nerve and various bodily functions. They delve into the complexities of the nervous system, exploring the intricate pathways and signaling mechanisms that contribute to vagus nerve disorders. By analyzing the patient’s symptoms and conducting thorough examinations, neurologists can identify the underlying causes of vagus nerve dysfunction and develop personalized treatment plans.
Furthermore, neurologists may collaborate with other specialists, such as gastroenterologists and cardiologists, to ensure a comprehensive approach to care. This interdisciplinary collaboration allows for a more holistic understanding of the patient’s condition and facilitates the development of tailored treatment strategies.
Gastroenterologists and Vagus Nerve Disorders
Gastroenterologists are physicians who specialize in disorders of the gastrointestinal (GI) tract and related organs. As the vagus nerve plays a crucial role in regulating digestive functions, gastroenterologists are well-equipped to diagnose and treat GI symptoms associated with vagus nerve disorders. They can perform specialized tests, such as esophageal manometry or gastric emptying studies, to evaluate the function of the GI tract and determine the underlying cause of gastrointestinal symptoms.
When it comes to vagus nerve disorders, gastroenterologists focus on understanding the intricate relationship between the vagus nerve and the digestive system. They explore how vagus nerve dysfunction can lead to a wide range of gastrointestinal symptoms, such as difficulty swallowing, acid reflux, bloating, and abdominal pain. By utilizing their expertise in gastroenterology, these specialists can provide targeted interventions to alleviate these symptoms and improve the overall quality of life for individuals with vagus nerve disorders.
Moreover, gastroenterologists may collaborate with neurologists and other specialists to ensure a comprehensive approach to care. By working together, they can address both the neurological and gastrointestinal aspects of vagus nerve disorders, providing patients with a more comprehensive and effective treatment plan.
Cardiologists and Vagus Nerve Disorders
Cardiologists are medical professionals specializing in heart and cardiovascular system disorders. Since the vagus nerve contributes to heart rate regulation, cardiologists are vital in identifying and managing cardiac symptoms associated with vagus nerve disorders. They may conduct tests like electrocardiograms (ECGs), stress tests, or echocardiograms to evaluate heart function and determine the appropriate treatment plan.
When it comes to vagus nerve disorders, cardiologists focus on understanding the intricate interplay between the vagus nerve and the cardiovascular system. They explore how vagus nerve dysfunction can lead to various cardiac symptoms, such as irregular heart rhythms, rapid heartbeats, or fluctuations in blood pressure. By utilizing their expertise in cardiology, these specialists can develop tailored treatment strategies to address these symptoms and optimize cardiac function.
Furthermore, cardiologists may collaborate with neurologists and other specialists to ensure a comprehensive approach to care. By working together, they can address both the neurological and cardiovascular aspects of vagus nerve disorders, providing patients with a more comprehensive and effective treatment plan.
Diagnostic Procedures for Vagus Nerve Disorders
Accurate diagnosis of vagus nerve disorders is crucial to determine the most suitable treatment approach. Doctors may employ several diagnostic procedures to gather information about the individual’s condition.
When a patient presents with symptoms that may indicate a vagus nerve disorder, the first step in the diagnostic process is a thorough physical examination. During this examination, the doctor will assess various aspects of the patient’s health, including heart rate, blood pressure, neurological reflexes, and other relevant signs. These initial clues can provide valuable insights into the functioning of the vagus nerve and help guide further diagnostic tests.
In addition to the physical examination, obtaining a detailed medical history is an essential part of the diagnostic process. The doctor will ask the patient about their symptoms, including their duration and any potential triggers. This information is crucial in narrowing down the diagnosis and identifying potential underlying causes. By understanding the patient’s medical history, the doctor can better assess the likelihood of a vagus nerve disorder and determine the most appropriate diagnostic tests.
Imaging Tests for Vagus Nerve Disorders
In some cases, imaging tests may be necessary to further evaluate the vagus nerve and surrounding structures. Magnetic resonance imaging (MRI) and computed tomography (CT) scans are commonly used imaging techniques that can help identify structural abnormalities or tumors affecting the vagus nerve. These tests provide detailed images of the internal structures, allowing doctors to visualize any potential issues and make an accurate diagnosis.
During an MRI or CT scan, the patient lies on a table that slides into a large, cylindrical machine. The machine uses a combination of magnetic fields and radio waves (MRI) or X-rays (CT) to create detailed cross-sectional images of the body. These images can reveal any abnormalities or tumors that may be affecting the vagus nerve, providing valuable information for the diagnosis and treatment planning.
Electromyography and Nerve Conduction Studies
Electromyography (EMG) and nerve conduction studies (NCS) are valuable tools for evaluating nerve function, including the vagus nerve. These tests are often performed to assess the integrity and functionality of the nerves and muscles.
During an EMG, small electrodes are inserted into the muscles being tested. These electrodes detect the electrical activity of the muscles, allowing the doctor to evaluate the function of the nerves that control them. By analyzing the electrical signals, the doctor can determine if there are any abnormalities in the nerve-muscle communication, which may indicate a vagus nerve disorder.
Nerve conduction studies, on the other hand, involve the application of small electrical shocks to the nerves. These shocks stimulate the nerves, and the response is recorded. By measuring the speed and strength of the nerve signals, the doctor can assess the functionality of the vagus nerve and identify any potential issues.
Both EMG and NCS are safe and non-invasive procedures that provide valuable information about the functioning of the vagus nerve. They can help diagnose various vagus nerve disorders, such as vagus nerve damage, compression, or dysfunction.
Treatment Options for Vagus Nerve Disorders
After a comprehensive evaluation, doctors can recommend appropriate treatment options tailored to the specific vagus nerve disorder and the individual’s symptoms and overall health. Treatment approaches may vary depending on the severity and underlying cause of the condition.
Vagus nerve disorders can be complex and challenging to manage, requiring a multidisciplinary approach involving various medical specialists. Neurologists, gastroenterologists, and cardiologists play essential roles in the care of individuals with vagus nerve disorders, leveraging their expertise to address specific aspects of the condition.
Medication and Vagus Nerve Disorders
Pharmacological interventions aim to manage symptoms and potentially modify the progression of vagus nerve disorders. Medications like anti-inflammatory drugs, pain relievers, proton pump inhibitors, or medications targeting specific symptoms, such as antiemetics or anticholinergics, may be prescribed based on the individual’s needs and treatment goals.
Anti-inflammatory drugs, such as corticosteroids, can help reduce inflammation and alleviate symptoms associated with vagus nerve disorders. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be prescribed to manage pain and discomfort. Proton pump inhibitors can be used to reduce stomach acid production, which can be beneficial for individuals with vagus nerve disorders that affect the gastrointestinal system.
In some cases, medications targeting specific symptoms may be prescribed. For example, antiemetics can help alleviate nausea and vomiting, while anticholinergics can help reduce excessive sweating or excessive salivation.
Surgical Interventions for Vagus Nerve Disorders
In certain cases, surgical interventions may be necessary to address underlying structural abnormalities or relieve nerve compression affecting the vagus nerve. Surgical options may include nerve decompression procedures, resection of tumors or growths, or the implantation of medical devices specifically designed to modulate vagus nerve activity.
Nerve decompression procedures involve relieving pressure on the vagus nerve by removing or repositioning surrounding tissues or structures that may be compressing the nerve. This can help alleviate symptoms and improve nerve function.
Resection of tumors or growths may be necessary if they are causing compression or damage to the vagus nerve. Surgical removal of these abnormal growths can help restore normal nerve function and alleviate symptoms.
For individuals with severe or refractory vagus nerve disorders, the implantation of medical devices may be considered. These devices, such as vagus nerve stimulators, can deliver electrical impulses to the vagus nerve, helping to regulate its activity and potentially reduce symptoms.
Lifestyle Changes and Vagus Nerve Disorders
In addition to medical interventions, incorporating lifestyle changes can significantly impact the management and overall well-being of individuals with vagus nerve disorders. These may include stress reduction techniques, dietary modifications, regular exercise, and proper sleep hygiene.
Stress reduction techniques, such as mindfulness meditation, deep breathing exercises, or yoga, can help individuals manage stress levels, which may contribute to symptom exacerbation. Dietary modifications, such as avoiding trigger foods or following a low-acid diet, can help reduce gastrointestinal symptoms associated with vagus nerve disorders.
Regular exercise has been shown to have numerous benefits for overall health and can help improve symptoms associated with vagus nerve disorders. Engaging in activities like walking, swimming, or cycling can help promote cardiovascular health and enhance overall well-being.
Proper sleep hygiene is also important for individuals with vagus nerve disorders. Establishing a regular sleep schedule, creating a comfortable sleep environment, and practicing relaxation techniques before bed can help improve sleep quality and promote overall health.
In summary, vagus nerve disorders require a multidisciplinary approach for accurate diagnosis and comprehensive treatment. Neurologists, gastroenterologists, and cardiologists play essential roles in the care of individuals with vagus nerve disorders, leveraging their expertise to address specific aspects of the condition. Diagnostic procedures such as physical examinations, imaging tests, and electromyography can aid in diagnosis, while treatment options range from medications to surgical interventions and lifestyle modifications. By seeking appropriate medical care and working collaboratively with healthcare professionals, individuals can embark on a journey toward improved quality of life and symptom management.