The vagus nerve, also known as the 10th cranial nerve, plays a crucial role in the regulation of various bodily functions, including digestion. Understanding the impact of vagus nerve disorders on digestion is essential for identifying and effectively managing these conditions. This article aims to provide an overview of the vagus nerve and its functions, discuss different vagus nerve disorders, examine the relationship between the vagus nerve and digestion, explore treatment options, and shed light on future developments in vagus nerve research.
An Overview of the Vagus Nerve and Its Functions
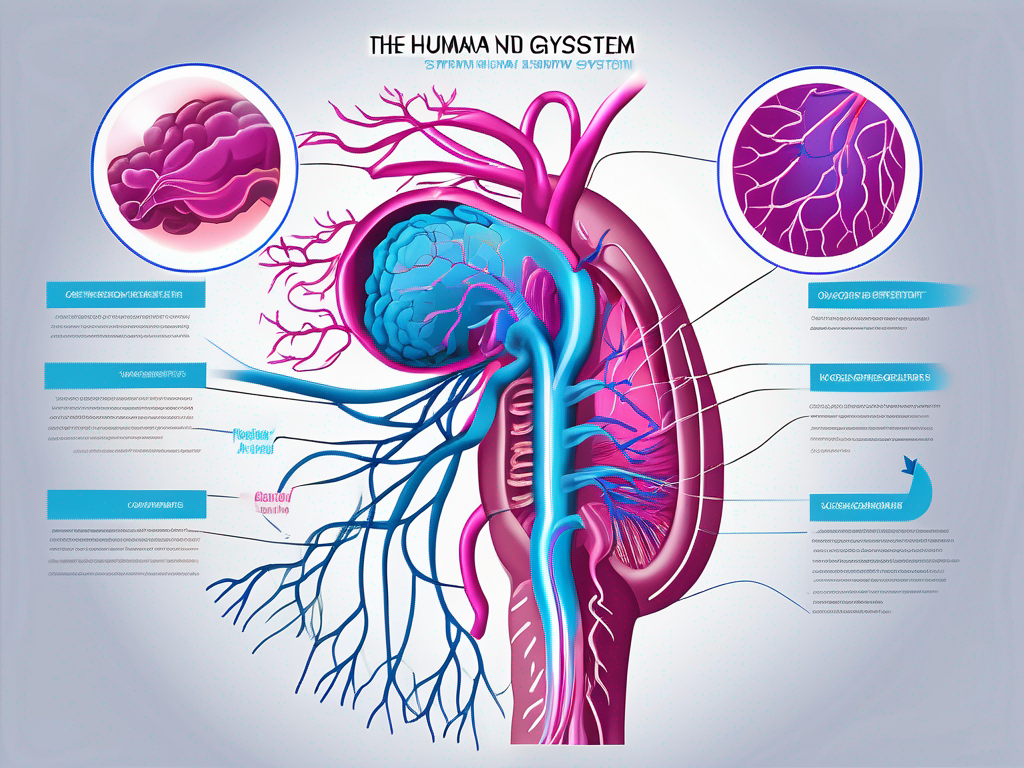
The vagus nerve is the longest of the cranial nerves and extends from the brainstem to various organs in the body, including the heart, lungs, stomach, and intestines. It plays a vital role in regulating several bodily functions, such as heart rate, respiration, and digestion.
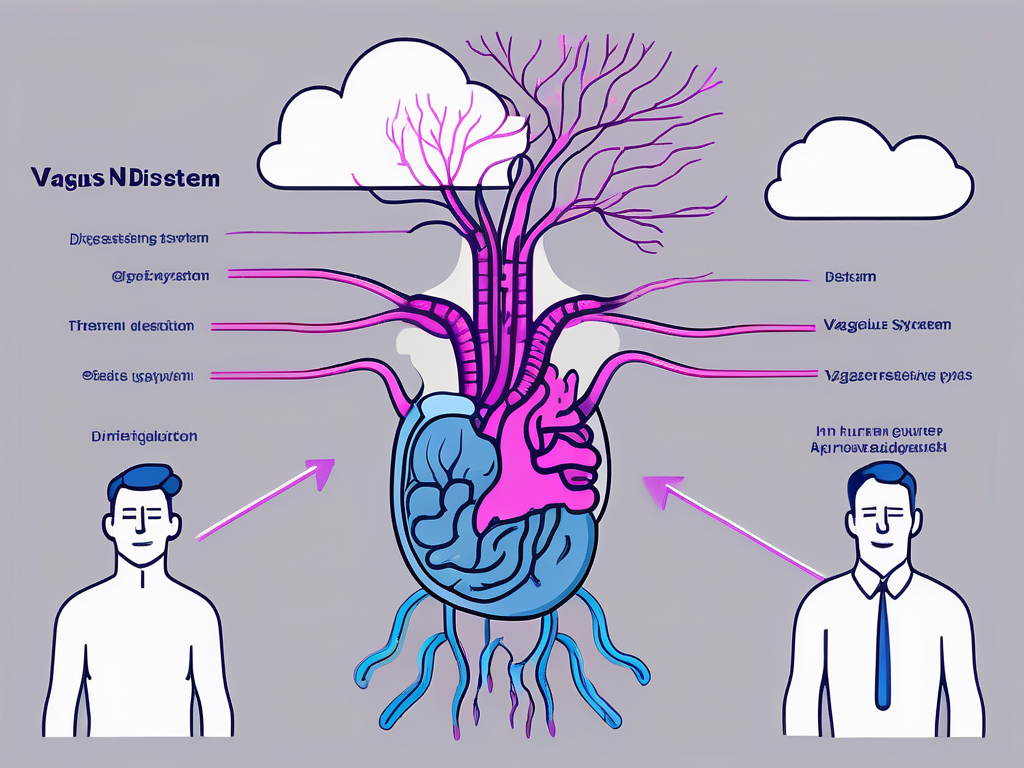
The vagus nerve consists of sensory and motor fibers, allowing it to transmit information from the organs to the brain and control the movements of various muscles. It is responsible for the parasympathetic nervous system’s actions, which promote rest, relaxation, and digestion.
The Anatomy of the Vagus Nerve
The vagus nerve originates in the medulla oblongata, which is located at the base of the brain. From there, it extends down the neck, chest, and abdomen, branching out to innervate different organs. The vagus nerve has both afferent (sensory) and efferent (motor) fibers that enable it to transmit signals bidirectionally.
In the gastrointestinal system, the vagus nerve innervates the esophagus, stomach, liver, gallbladder, pancreas, and intestines. This extensive network of connections allows the vagus nerve to regulate digestion and nutrient absorption efficiently.
For example, when you eat a meal, the vagus nerve is responsible for sending signals to the brain to initiate the release of digestive enzymes and hormones necessary for breaking down food. It also stimulates the production of gastric acid, which aids in the digestion of proteins and other nutrients.
Furthermore, the vagus nerve plays a crucial role in regulating intestinal peristalsis, the wave-like contractions that facilitate the movement of food through the digestive tract. These coordinated contractions ensure that food is properly propelled through the esophagus, stomach, and intestines, allowing for efficient nutrient absorption.
The Role of the Vagus Nerve in the Body
The vagus nerve is responsible for maintaining homeostasis in the body by regulating various physiological processes. One of its primary functions is to initiate the rest and digest response, which allows the body to focus on digestion and nutrient absorption.
When activated, the vagus nerve promotes a state of relaxation, reducing heart rate and blood pressure. This response is essential for optimal digestion, as it diverts blood flow away from the muscles and towards the digestive organs, ensuring they receive adequate oxygen and nutrients.
Additionally, the vagus nerve influences the gut-brain axis, a bidirectional communication system between the gut and the brain. This connection ensures proper coordination between the digestive system and the central nervous system, facilitating optimal digestive function.
Moreover, recent research has shown that the vagus nerve also plays a role in modulating inflammation. It has anti-inflammatory effects and can help regulate the immune response, protecting the body from excessive inflammation that can lead to various diseases.
In conclusion, the vagus nerve is a crucial component of the autonomic nervous system, responsible for regulating various physiological processes, particularly those related to digestion and homeostasis. Its extensive network of connections and bidirectional signaling make it a vital player in maintaining overall health and well-being.
Understanding Vagus Nerve Disorders
Vagus nerve disorders can disrupt the normal functioning of this vital nerve, leading to various health issues. Recognizing the different types of vagus nerve disorders and understanding their symptoms and diagnosis are crucial for proper management and treatment.
Common Vagus Nerve Disorders
There are several vagus nerve disorders, each with its specific impact on bodily functions. Some common vagus nerve disorders include vagus nerve compression, vagus nerve injury, and vagus nerve dysfunction.
Vagus nerve compression occurs when nearby structures, such as tumors or blood vessels, exert pressure on the nerve, impeding its function. This compression can result in a range of symptoms, including difficulty swallowing, hoarseness, and a weak voice. In severe cases, it can even lead to problems with heart rate and blood pressure regulation.
Vagus nerve injury can result from trauma, surgery, or infections affecting the nerve. Injuries to the vagus nerve can cause a variety of symptoms, depending on the extent and location of the damage. These symptoms may include difficulty speaking or swallowing, a weak cough, and problems with digestion.
Vagus nerve dysfunction may arise due to underlying medical conditions, such as diabetes or autoimmune diseases. When the vagus nerve is not functioning properly, it can lead to a range of symptoms, including heart palpitations, digestive issues, and difficulty regulating body temperature.
Symptoms and Diagnosis of Vagus Nerve Disorders
Recognizing the symptoms of vagus nerve disorders is essential for an accurate diagnosis. These disorders can manifest through a variety of symptoms, including digestive problems, such as bloating, nausea, vomiting, and changes in bowel movements.
In addition to digestive symptoms, vagus nerve disorders can also cause issues with heart rate and blood pressure regulation. Some individuals may experience a rapid heart rate or low blood pressure, while others may have fluctuations in heart rate and blood pressure throughout the day.
Diagnosing vagus nerve disorders often requires a thorough medical evaluation that may include a review of symptoms, physical examination, and diagnostic tests. During the physical examination, a healthcare provider may check for signs of nerve damage, such as muscle weakness or decreased reflexes.
Imaging techniques, such as MRI or ultrasound, can help identify structural abnormalities or compression on the vagus nerve. These imaging tests provide detailed images of the nerve and surrounding structures, allowing healthcare professionals to assess any potential issues.
Additionally, specialized tests, like an esophageal manometry or an electrogastrogram, may provide further insight into the nerve’s functionality. An esophageal manometry measures the strength and coordination of the muscles in the esophagus, which can be affected by vagus nerve disorders. An electrogastrogram measures the electrical activity of the stomach, providing information about its motility and function.
Overall, understanding vagus nerve disorders and their symptoms is essential for early detection and appropriate treatment. If you suspect you may have a vagus nerve disorder, it is important to consult with a healthcare professional for a comprehensive evaluation and personalized care plan.
The Vagus Nerve and Digestion
The vagus nerve’s influence on digestion is significant, as it orchestrates the complex processes involved in breaking down food, absorbing nutrients, and eliminating waste. Understanding its role in digestion and how vagus nerve disorders can disrupt these functions is essential for managing related gastrointestinal issues.
The Vagus Nerve’s Role in Digestion
The vagus nerve plays a crucial role in coordinating the various stages of digestion. It stimulates the release of gastric acid, promotes the contraction of smooth muscles in the stomach and intestines, and triggers the release of digestive enzymes and hormones.
When food enters the stomach, the vagus nerve is responsible for signaling the release of gastric acid. This acid is vital for breaking down proteins and activating digestive enzymes. Without the vagus nerve’s stimulation, the stomach may not produce enough acid, leading to poor digestion and nutrient absorption.
In addition to acid secretion, the vagus nerve also controls the contraction of smooth muscles in the stomach and intestines. These contractions help mix food with digestive enzymes and propel it through the digestive tract. Without proper vagal stimulation, these contractions may become weak or irregular, causing food to move slowly through the digestive system.
Furthermore, the vagus nerve plays a crucial role in triggering the release of digestive enzymes and hormones. Enzymes such as amylase, lipase, and protease are essential for breaking down carbohydrates, fats, and proteins, respectively. Hormones like gastrin, cholecystokinin, and secretin regulate various aspects of digestion, including gastric acid secretion, bile release, and pancreatic enzyme production.
Additionally, the vagus nerve influences the pyloric sphincter’s activity, controlling the passage of food from the stomach to the small intestine. It also modulates the enteric nervous system, a network of neurons within the gastrointestinal system that helps regulate digestion.
How Vagus Nerve Disorders Affect Digestion
When vagus nerve disorders disrupt the nerve’s normal function, various digestive problems can arise. For instance, reduced vagal tone, commonly seen in conditions like gastroparesis, slows down gastric motility, leading to delayed emptying of food from the stomach.
Gastroparesis, a condition characterized by delayed stomach emptying, can cause symptoms such as nausea, vomiting, bloating, and early satiety. The vagus nerve’s impaired function in gastroparesis prevents the stomach from contracting effectively, resulting in food remaining in the stomach for longer periods than usual.
Other vagus nerve disorders can cause aberrant signaling between the vagus nerve and the central nervous system, leading to dysregulation of digestive functions. This can result in symptoms like heartburn, bloating, abdominal pain, and altered bowel movements.
Furthermore, vagus nerve disorders can disrupt the coordination between the vagus nerve and the enteric nervous system. This disruption can lead to irregularities in digestive processes, such as impaired nutrient absorption, imbalanced gut microbiota, and altered intestinal motility.
Overall, understanding the intricate relationship between the vagus nerve and digestion is crucial for managing gastrointestinal issues. By addressing vagus nerve disorders and promoting optimal vagal tone, healthcare professionals can help restore normal digestive functions and improve overall gastrointestinal health.
Treatment and Management of Vagus Nerve Disorders
Effectively managing vagus nerve disorders requires a comprehensive approach that addresses the underlying cause, alleviates symptoms, and supports overall vagus nerve health. Treatment options may vary depending on the specific disorder and its severity.
Vagus nerve disorders can be challenging to manage, but with the right treatment and lifestyle changes, individuals can experience significant improvements in their symptoms and overall well-being.
Medical Treatments for Vagus Nerve Disorders
Medical interventions for vagus nerve disorders aim to address the underlying cause and manage symptoms. Treatment options may include medications to control inflammation, manage pain, or enhance nerve function. In some cases, surgical interventions, such as nerve decompression or neurostimulation, may be necessary to relieve pressure on the vagus nerve.
When it comes to medication, healthcare professionals may prescribe anti-inflammatory drugs to reduce inflammation around the vagus nerve. These medications can help alleviate pain and discomfort associated with vagus nerve disorders. Additionally, nerve-specific medications may be prescribed to enhance nerve function and promote healing.
In more severe cases, surgical interventions may be considered. Nerve decompression surgery involves relieving pressure on the vagus nerve by removing any surrounding structures that may be compressing it. This procedure can provide long-term relief for individuals with chronic vagus nerve disorders.
Another surgical option is neurostimulation, which involves implanting a device that delivers electrical impulses to the vagus nerve. This technique can help regulate nerve activity and reduce symptoms such as pain, nausea, and digestive issues.
Lifestyle Changes to Improve Vagus Nerve Health
Adopting a healthy lifestyle can also contribute to vagus nerve health and overall well-being. Engaging in stress-reducing activities, such as meditation or yoga, can help regulate the autonomic nervous system and maintain optimal vagal tone.
Regular meditation practice has been shown to activate the relaxation response, which can help reduce stress and promote vagus nerve function. Yoga, on the other hand, combines physical postures, breathing exercises, and meditation, making it a holistic practice that can benefit both the mind and body.
In addition to stress reduction techniques, maintaining a balanced diet is crucial for vagus nerve health. A diet rich in fiber, such as fruits, vegetables, and whole grains, can support healthy digestion and promote optimal vagus nerve function. Avoiding processed foods, which are often high in unhealthy fats and sugars, is also important as they can contribute to inflammation and nerve damage.
Hydration is another key factor in supporting vagus nerve health. Drinking an adequate amount of water throughout the day helps maintain proper nerve function and ensures optimal hydration of the body’s tissues.
Regular exercise is not only beneficial for overall health but also plays a vital role in maintaining optimal nerve function. Engaging in moderate-intensity aerobic activities, such as walking, swimming, or cycling, can help improve blood circulation and promote nerve health.
Lastly, getting enough quality sleep is essential for the body’s overall healing and repair processes, including nerve regeneration. Aim for 7-9 hours of uninterrupted sleep each night to support vagus nerve health and overall well-being.
The Future of Vagus Nerve Research
Research on the vagus nerve is an active area of study, with ongoing efforts to deepen our understanding of its functions and develop innovative treatments for vagus nerve disorders. Advancements in this field hold the promise of improving the management and outcomes of individuals affected by these conditions.
Current Research on Vagus Nerve Disorders
Scientists are exploring various aspects of vagus nerve disorders, ranging from understanding the underlying mechanisms to evaluating novel therapies. Current research aims to identify genetic factors that contribute to vagus nerve disorders, develop targeted treatments, and explore the potential of bioelectronic medicine in modulating vagus nerve activity.
Potential Future Developments in Vagus Nerve Treatment
As research progresses, exciting developments in vagus nerve treatment may emerge. Novel therapies, such as vagus nerve stimulation and bioelectronic implants, show promise in modulating nerve activity and restoring normal function. These advancements may offer new hope for individuals with treatment-resistant vagus nerve disorders.
In conclusion, understanding the impact of vagus nerve disorders on digestion is crucial for identifying and effectively managing these conditions. The vagus nerve’s role in digestion is extensive, and disruptions to its normal functioning can lead to various gastrointestinal problems. Proper diagnosis, treatment, and lifestyle modifications can help mitigate the effects of vagus nerve disorders on digestion and improve overall well-being. Ongoing research in this field holds the potential to revolutionize vagus nerve disorder management and offer new avenues for treatment.