The vagus nerve, a crucial component of the autonomic nervous system, plays a vital role in regulating various bodily functions. It meanders through the body, connecting the brainstem to a range of organs, including the heart, lungs, and digestive system. In this article, we will delve into the intricacies of vagus nerve disorders in the thoracic region, exploring their implications, causes, and treatment options.
Anatomy of the Vagus Nerve
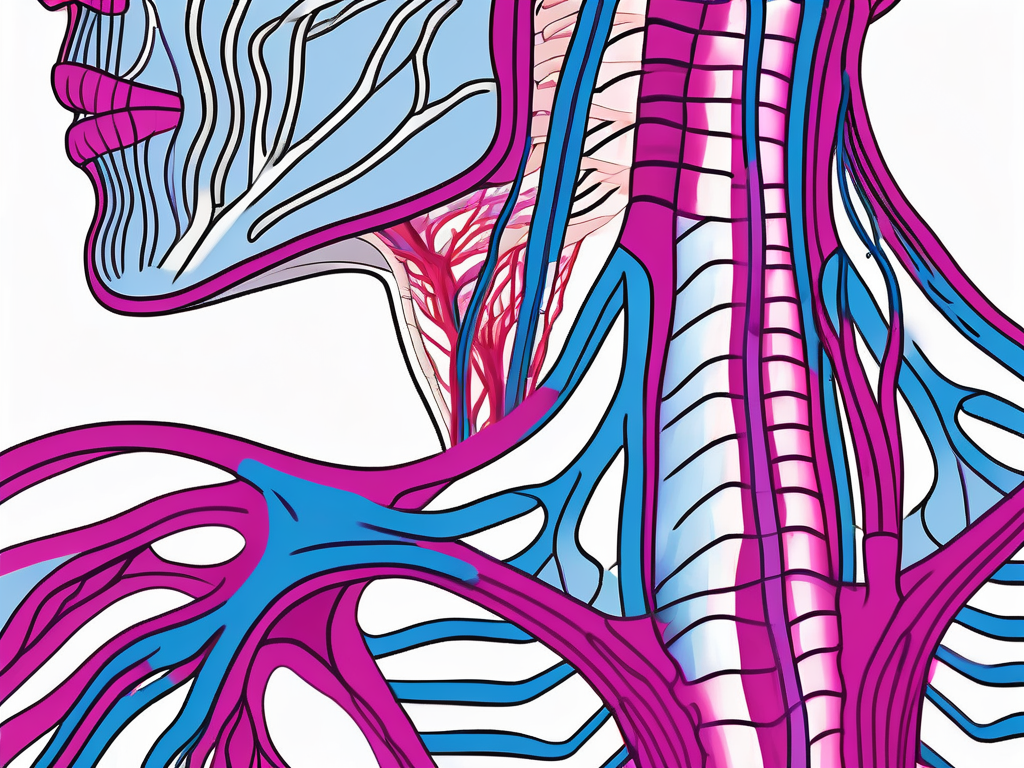
The vagus nerve, also known as the cranial nerve X, is a long, wandering nerve that originates in the medulla oblongata, a region of the brainstem. It extends down through the neck and into the chest and abdomen, exerting its influence on numerous bodily functions along the way. The vagus nerve comprises both sensory and motor fibers, allowing for bidirectional communication between the brain and various organ systems.
The Vagus Nerve and its Functions
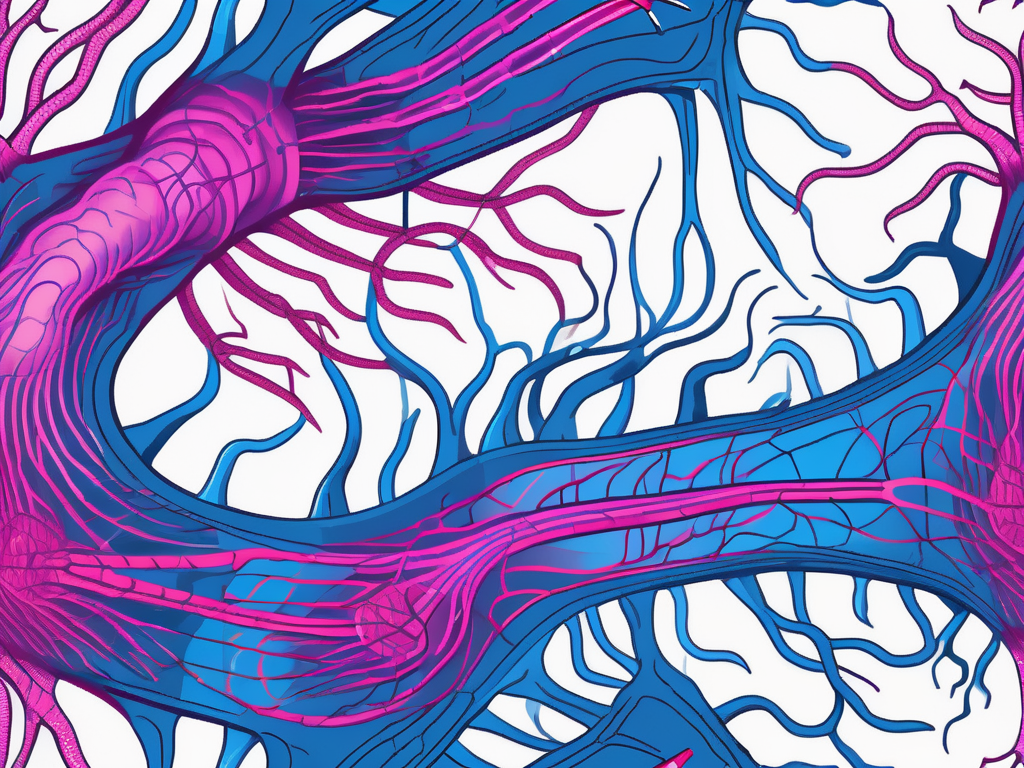
One of the vagus nerve’s primary functions is to regulate the parasympathetic nervous system. Through its extensive network of branches, it controls essential bodily functions such as heart rate, digestion, and respiration. Additionally, the vagus nerve plays a role in regulating inflammation and immune response, highlighting its crucial influence on overall health and wellbeing.
Location and Pathway of the Vagus Nerve
The vagus nerve follows a complex pathway throughout the body. It descends from the brainstem, passing through the neck’s carotid sheath, adjacent to the common carotid artery and internal jugular vein. From there, it navigates into the thoracic region, looping around the aortic arch and forming connections with the heart and lungs. Continuing its journey, the vagus nerve extends into the abdomen, innervating organs such as the stomach, liver, and intestines.
As the vagus nerve travels through the neck, it sends branches to various structures along its path. One of these branches, known as the superior laryngeal nerve, innervates the muscles responsible for controlling the vocal cords. This intricate connection allows for precise control over speech and voice modulation.
Within the thoracic region, the vagus nerve forms connections with the heart, playing a vital role in regulating heart rate and rhythm. It sends signals to the sinoatrial node, the natural pacemaker of the heart, ensuring that the heart beats at a steady pace. Additionally, the vagus nerve influences the contraction and relaxation of the smooth muscles in the lungs, facilitating the process of respiration.
As the vagus nerve extends into the abdomen, it continues to exert its influence on various organs. It innervates the stomach, playing a role in regulating gastric acid secretion and motility. The liver also receives input from the vagus nerve, allowing for the modulation of bile production and release. Furthermore, the vagus nerve controls the movement and absorption of nutrients in the intestines, contributing to the digestive process.
Aside from its role in regulating bodily functions, the vagus nerve has been linked to mental health and emotional well-being. Studies have shown that stimulating the vagus nerve can have a calming effect on the brain, reducing anxiety and improving mood. This connection between the vagus nerve and mental health highlights the intricate relationship between the nervous system and emotional states.
In conclusion, the vagus nerve is a remarkable structure that extends throughout the body, connecting the brain to various organ systems. Its functions encompass the regulation of heart rate, digestion, respiration, inflammation, and immune response. Understanding the anatomy and functions of the vagus nerve provides insight into the intricate connections between the brain and the body, highlighting the importance of this nerve in maintaining overall health and well-being.
The Connection between the Vagus Nerve and the Thoracic Region
Within the thoracic region, the vagus nerve assumes a significant role in maintaining proper functioning. Its intricate connections with the heart and lungs contribute to cardiovascular stability and respiratory regulation. Let us explore how the vagus nerve influences thoracic health and how the thoracic region, in turn, affects the vagus nerve.
The vagus nerve plays a critical role in maintaining cardiovascular health within the thoracic region. It coordinates heart rate and rhythm, ensuring efficient blood flow to meet the body’s demands. This intricate network of nerve fibers extends from the brainstem down to the thoracic region, where it branches out to innervate various structures.
One of the primary functions of the vagus nerve in the thoracic region is to regulate heart rate. Through its parasympathetic influence, the vagus nerve helps to slow down the heart rate during periods of rest and relaxation. This mechanism is crucial in maintaining a healthy cardiovascular system, as it prevents the heart from overworking itself.
In addition to heart rate regulation, the vagus nerve also plays a role in rhythm control. It helps to synchronize the electrical impulses that coordinate the contraction and relaxation of the heart muscles. This synchronization ensures that the heart functions efficiently, pumping blood throughout the body in a coordinated manner.
Moreover, the vagus nerve interacts with the pulmonary system, modulating bronchial constriction, and influencing respiratory rate. By sending signals to the smooth muscles surrounding the bronchial tubes, the vagus nerve helps to regulate the diameter of the airways. This control is essential in preventing excessive constriction or dilation of the bronchial tubes, ensuring optimal airflow to the lungs.
Furthermore, the vagus nerve influences respiratory rate. It helps to regulate the depth and frequency of breathing, ensuring that the body receives an adequate supply of oxygen. By adjusting the rate of breathing, the vagus nerve helps to maintain the balance between oxygen intake and carbon dioxide elimination, optimizing respiratory function.
Conversely, thoracic health exerts a significant impact on the vagus nerve’s functionality. Conditions such as thoracic inflammation, infections, or structural abnormalities can impinge on the vagus nerve, affecting its ability to transmit signals efficiently. Inflammation within the thoracic region can lead to nerve compression or irritation, disrupting the normal flow of information along the vagus nerve.
Furthermore, thoracic pathologies, such as cardiac arrhythmias or chronic lung diseases, can disrupt the delicate balance maintained by the vagus nerve, consequently compromising overall health. For example, in conditions like atrial fibrillation, an abnormal heart rhythm, the vagus nerve may become overactive or underactive, leading to further irregularities in heart rate and rhythm.
In conclusion, the vagus nerve and the thoracic region have a complex and interdependent relationship. The vagus nerve plays a crucial role in maintaining cardiovascular stability and respiratory regulation within the thoracic region. Simultaneously, the health of the thoracic region, including the heart and lungs, can significantly impact the functionality of the vagus nerve. Understanding this connection is essential for managing and treating various thoracic complications and maintaining overall health.
Common Vagus Nerve Disorders
Vagus nerve disorders encompass a wide spectrum of conditions that can disrupt the nerve’s normal functioning. Ranging from mild to severe, these disorders can create a host of symptoms and complications. Understanding the symptoms, diagnosis, causes, and risk factors associated with vagus nerve disorders is crucial in ensuring early intervention and appropriate management.
Symptoms and Diagnosis of Vagus Nerve Disorders
The manifestations of vagus nerve disorders can vary widely, depending on the specific condition impacting the nerve. Patients may experience symptoms such as heart palpitations, dizziness, difficulty swallowing, or gastrointestinal disturbances. These symptoms can be distressing and significantly impact an individual’s quality of life.
Diagnosing vagus nerve disorders often involves a comprehensive evaluation of medical history, symptom assessment, and clinical examinations. Healthcare professionals may inquire about the frequency and duration of symptoms, as well as any triggers or patterns that may be present. Physical examinations may include tests to assess heart rate variability, blood pressure changes, or reflex responses.
In some cases, diagnostic tests such as nerve conduction studies or imaging modalities may be utilized to further evaluate the functioning of the vagus nerve. Nerve conduction studies involve measuring the electrical activity of the nerve, providing valuable information about its integrity and responsiveness. Imaging modalities, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, can help identify any structural abnormalities or potential sources of nerve compression.
Causes and Risk Factors for Vagus Nerve Disorders
Vagus nerve disorders can arise from a multitude of causes and risk factors. Structural abnormalities within the nerve, such as compressions or entrapments, can impede its functionality. These abnormalities may be congenital or acquired, resulting from trauma, tumors, or other underlying conditions.
Inflammatory conditions, autoimmune diseases, or infections can also lead to vagus nerve dysfunction. Conditions such as diabetes, Lyme disease, or Guillain-Barré syndrome have been associated with vagus nerve disorders. Inflammation or damage to the nerve can disrupt its normal signaling pathways, leading to a wide range of symptoms.
Additionally, lifestyle factors can play a role in the development of vagus nerve disorders. Chronic stress, for example, can have a detrimental effect on the nervous system, including the vagus nerve. Prolonged stress can lead to dysregulation of the autonomic nervous system, which the vagus nerve is a part of, potentially contributing to the development of disorders.
Poor diet and sedentary habits can also increase the risk of developing vagus nerve disorders. A diet lacking in essential nutrients can negatively impact nerve health and function. Regular physical activity, on the other hand, promotes overall well-being and supports optimal nerve function.
It is important to note that while these causes and risk factors are associated with vagus nerve disorders, each individual’s experience may vary. Consulting with a healthcare professional is essential for accurate diagnosis and tailored management strategies.
Treatment Options for Vagus Nerve Disorders
Effectively managing vagus nerve disorders is crucial in optimizing patient outcomes and improving quality of life. Treatment approaches typically involve a multidimensional approach, encompassing medical interventions, therapeutic procedures, lifestyle modifications, and self-care practices.
Vagus nerve disorders can manifest in various ways, leading to symptoms such as irregular heart rate, digestive issues, and even mental health conditions. Therefore, it is essential to tailor the treatment plan to the specific needs of each individual patient.
Medical Treatments and Procedures
Medical interventions for vagus nerve disorders may include medications to alleviate symptoms, regulate heart rate, or modulate inflammation. These medications can target specific receptors in the body to restore balance and improve nerve function. However, it is important to note that medication alone may not be sufficient and should be combined with other treatment modalities for optimal results.
In some cases, surgical procedures may be necessary to address anatomical abnormalities or relieve nerve entrapment. For example, if the vagus nerve is compressed by surrounding structures, a surgical intervention may be required to release the pressure and restore proper nerve function. These procedures are typically performed by highly skilled surgeons with expertise in neurology and can significantly improve the patient’s quality of life.
Close collaboration between patients and healthcare providers is essential in determining the most suitable treatment plan. Regular follow-up appointments and open communication allow for adjustments to be made based on the patient’s progress and response to treatment.
Lifestyle Changes and Home Remedies
Complementary to medical treatments, making significant lifestyle changes can support vagus nerve health and overall well-being. Engaging in regular physical exercise not only improves cardiovascular health but also stimulates the vagus nerve, promoting its proper functioning. Activities such as yoga, tai chi, and swimming have been shown to have a positive impact on nerve health and can be incorporated into the patient’s daily routine.
Adopting stress-reducing techniques such as meditation or deep breathing exercises can also have a profound effect on vagus nerve disorders. These practices activate the body’s relaxation response, reducing stress hormones and promoting a sense of calm. Additionally, maintaining a balanced diet rich in nutrients, antioxidants, and omega-3 fatty acids can support nerve health and reduce inflammation in the body.
Moreover, certain home remedies, such as herbal supplements or acupuncture, may offer additional benefits, but their efficacy should be further studied and evaluated. It is important to consult with a healthcare professional before incorporating any alternative therapies into the treatment plan to ensure their safety and effectiveness.
In conclusion, treating vagus nerve disorders requires a comprehensive approach that combines medical interventions, therapeutic procedures, lifestyle modifications, and self-care practices. By addressing the underlying causes and promoting nerve health, patients can experience improved symptoms, enhanced well-being, and a better quality of life.
The Future of Vagus Nerve Disorder Research
The field of vagus nerve disorder research is continuously evolving, promising new insights and therapeutic possibilities. Ongoing studies aim to unveil the intricacies of vagus nerve functioning, propose innovative treatment modalities, and explore the potential of emerging therapies.
Emerging Treatments and Therapies
Researchers are investigating novel approaches to tackle vagus nerve disorders, ranging from advanced surgical techniques to neuromodulation therapies. Initiatives focused on harnessing the benefits of bioelectronic devices and implanted stimulators show promising results in managing conditions such as epilepsy, depression, or inflammatory diseases. These exciting developments hold the potential to revolutionize vagus nerve disorder treatment.
The Importance of Continued Research
Continued research in the realm of vagus nerve disorders is crucial in unraveling the complexities of these conditions and developing effective interventions. By deepening our understanding of the vagus nerve’s intricacies and exploring the interplay between thoracic health and nerve functioning, researchers can pave the way for innovative therapies and improved patient outcomes.
In conclusion, understanding vagus nerve disorders in the thoracic region requires delving into the anatomy, functions, and interdependencies of this crucial nerve. By recognizing the impact of thoracic health on vagus nerve functioning and vice versa, healthcare providers can develop comprehensive treatment plans aimed at alleviating symptoms and restoring balance. The future of vagus nerve disorder research holds immense potential, paving the way for groundbreaking therapies and optimizing patient care.