The vagus nerve is a vital component of the human body’s nervous system and plays a crucial role in regulating various bodily functions. When problems arise with the vagus nerve, seeking appropriate medical care is essential for diagnosis and treatment. In this article, we will explore the different types of doctors involved in treating vagus nerve disorders, the diagnostic process, treatment options, and the importance of follow-up care.
Understanding the Vagus Nerve and Its Functions
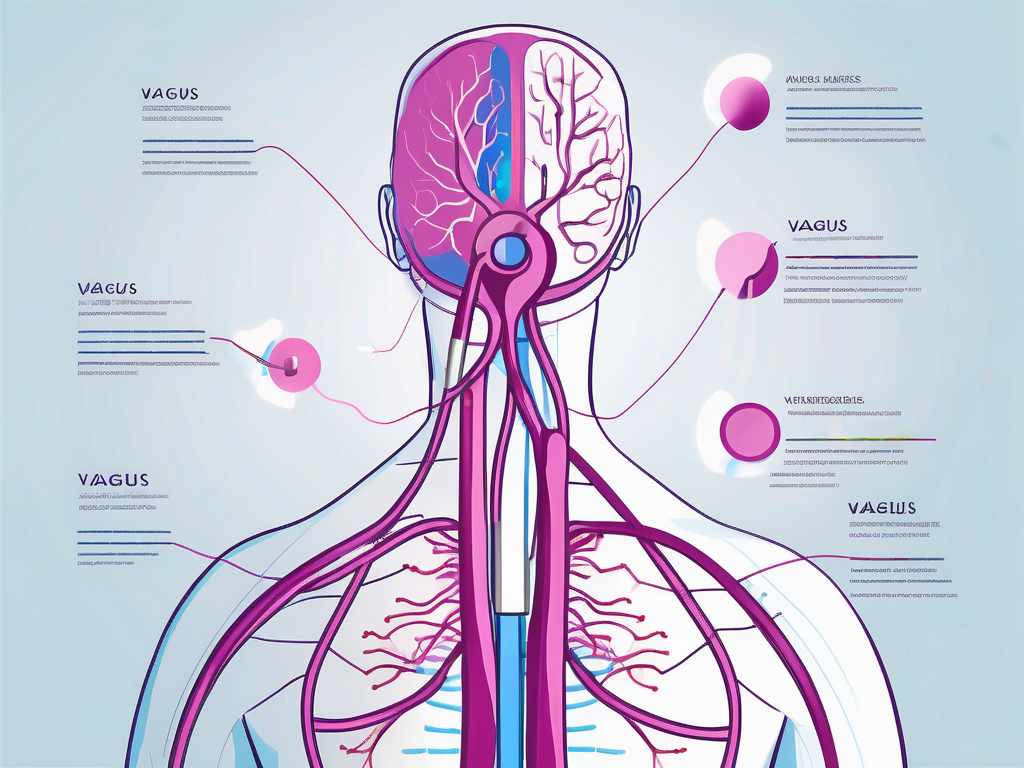
The vagus nerve is the longest cranial nerve in the body, running from the brainstem to the abdomen. It is responsible for transmitting signals between the brain and various organs, including the heart, lungs, digestive system, and throat. The vagus nerve is involved in regulating heart rate, breathing, digestion, and speech.
But let’s dive deeper into the fascinating world of the vagus nerve and explore its intricate functions.
The Role of the Vagus Nerve in the Body
As a key part of the parasympathetic nervous system, the vagus nerve helps to maintain balance and homeostasis in the body. It regulates the release of acetylcholine, a neurotransmitter that promotes relaxation and slows down bodily functions.
When the vagus nerve is activated, it sends signals to the heart, instructing it to beat at a slower pace. This helps to reduce heart rate and blood pressure, promoting a state of calmness and relaxation.
In addition to its cardiovascular effects, the vagus nerve also plays a crucial role in the respiratory system. It regulates breathing by controlling the muscles responsible for expanding and contracting the lungs. By stimulating the vagus nerve, we can enhance our breathing patterns and promote a sense of tranquility.
But the vagus nerve’s influence doesn’t stop there. It extends its reach to the digestive system, where it aids in the process of digestion. By stimulating the release of digestive enzymes and increasing blood flow to the gastrointestinal tract, the vagus nerve ensures that our bodies efficiently break down food and absorb essential nutrients.
Furthermore, the vagus nerve is intricately involved in speech production. It innervates the muscles responsible for controlling the vocal cords, allowing us to modulate our voices and communicate effectively.
Common Disorders Associated with the Vagus Nerve
Vagus nerve disorders can lead to a variety of symptoms and conditions. One such disorder is vagus nerve damage, which can occur due to trauma, surgery, or underlying medical conditions. Damage to the vagus nerve can disrupt its ability to transmit signals properly, leading to symptoms such as difficulty swallowing, hoarseness, and a rapid heart rate.
Another condition associated with the vagus nerve is vocal cord paralysis. When the vagus nerve is impaired, the muscles controlling the vocal cords may become weak or paralyzed, resulting in a change in voice quality and difficulty speaking.
Gastroparesis, a condition characterized by delayed stomach emptying, is also linked to vagus nerve dysfunction. When the vagus nerve fails to transmit signals effectively to the stomach muscles, food remains in the stomach for a longer time, causing symptoms like bloating, nausea, and vomiting.
Seizures, although complex and multifactorial, can also be influenced by the vagus nerve. Vagus nerve stimulation, a therapeutic approach, involves the use of electrical impulses to stimulate the vagus nerve and help reduce the frequency and severity of seizures in individuals with epilepsy.
Understanding the vagus nerve and its functions is essential for comprehending the intricate connections between our brain and body. By exploring the role of the vagus nerve in maintaining homeostasis and its involvement in various disorders, we gain a deeper appreciation for the complexity of our physiological systems.
The Different Types of Doctors Involved in Treating Vagus Nerve Disorders
Several medical specialists play a role in the diagnosis and treatment of vagus nerve disorders. These specialists possess expertise in areas related to the nervous system, otolaryngology, and gastroenterology.
Neurologists and the Nervous System
Neurologists are medical doctors who specialize in the diagnosis and treatment of disorders related to the nervous system. They are highly trained in evaluating and managing conditions affecting the vagus nerve, such as neuropathy, epilepsy, and autonomic dysfunction. Neurologists may conduct neurological exams, order diagnostic tests, and recommend appropriate treatment plans.
When it comes to vagus nerve disorders, neurologists are at the forefront of understanding the intricate workings of this crucial nerve. They have a deep understanding of the complex network of nerves that make up the nervous system and how they interact with the vagus nerve. Neurologists use their expertise to identify the root cause of vagus nerve disorders and develop personalized treatment plans for their patients.
Additionally, neurologists may collaborate with other specialists, such as neurosurgeons, to explore surgical interventions for severe cases of vagus nerve disorders. They work closely with their patients to monitor their progress and make any necessary adjustments to their treatment plans.
Otolaryngologists and Vagus Nerve Disorders
Otolaryngologists, commonly known as ear, nose, and throat (ENT) doctors, are specialists who focus on disorders of the head and neck. They play a crucial role in diagnosing and treating conditions that affect the vagus nerve in the throat and upper airway, such as vocal cord paralysis and dysphagia. Otolaryngologists may perform specialized procedures, including laryngoscopy and electromyography, to assess the function of the vagus nerve in these areas.
When it comes to vagus nerve disorders, otolaryngologists bring their expertise in the head and neck region to the table. They have a deep understanding of the anatomy and function of the vagus nerve in this area and can identify any abnormalities or dysfunctions that may be causing the patient’s symptoms.
In addition to their diagnostic role, otolaryngologists may also provide various treatment options for vagus nerve disorders. They may recommend voice therapy for patients with vocal cord paralysis or suggest surgical interventions to correct any structural issues that may be affecting the vagus nerve. Otolaryngologists work closely with their patients to ensure the best possible outcomes and improve their quality of life.
Gastroenterologists and the Vagus Nerve
Gastroenterologists specialize in the diagnosis and treatment of gastrointestinal disorders. They play a vital role in managing conditions such as gastroparesis, which can result from vagus nerve dysfunction. Gastroenterologists may perform tests such as gastric emptying studies and manometry to assess the function of the digestive system and formulate appropriate treatment plans.
When it comes to vagus nerve disorders, gastroenterologists focus on the impact of vagus nerve dysfunction on the digestive system. They understand the crucial role the vagus nerve plays in regulating digestion and can identify any disruptions or abnormalities that may be causing gastrointestinal symptoms.
Gastroenterologists work closely with their patients to develop personalized treatment plans that address the underlying cause of their vagus nerve disorder. They may recommend dietary changes, medications, or other interventions to manage symptoms and improve overall digestive function. Gastroenterologists also collaborate with other specialists, such as nutritionists, to provide comprehensive care for their patients.
The Diagnostic Process for Vagus Nerve Disorders
Diagnosing vagus nerve disorders involves a thorough evaluation of a patient’s medical history, symptoms, and physical examination. The diagnostic process typically consists of an initial consultation and the use of various diagnostic tests.
Initial Consultation and Symptoms Review
During the initial consultation, the doctor will review the patient’s symptoms and medical history. They will inquire about any previous diagnoses or treatments related to the vagus nerve. Understanding the nature and duration of symptoms helps the doctor determine the appropriate diagnostic approach.
The doctor may ask the patient about the specific symptoms they are experiencing, such as difficulty swallowing, voice changes, or gastrointestinal issues. They will also inquire about any factors that may exacerbate or alleviate the symptoms, such as stress or certain activities. By gathering this information, the doctor can gain insight into the potential underlying cause of the vagus nerve disorder.
In addition to reviewing the patient’s symptoms, the doctor will also perform a physical examination. This may involve assessing the patient’s reflexes, muscle strength, and sensation in various parts of the body. The doctor may also examine the patient’s throat and neck for any abnormalities that could be related to vagus nerve dysfunction.
Diagnostic Tests for Vagus Nerve Disorders
Diagnostic tests play a crucial role in identifying and assessing vagus nerve disorders. These tests help to confirm the presence of a vagus nerve disorder, determine its severity, and guide treatment decisions.
One common diagnostic test for vagus nerve disorders is nerve conduction studies. This test measures the speed and strength of electrical signals as they travel along the vagus nerve. By evaluating the conduction of these signals, doctors can determine if there are any abnormalities or disruptions in the nerve’s function.
Another test that may be used is electromyography (EMG). This test involves inserting small, thin needles into specific muscles to measure their electrical activity. By analyzing the muscle response, doctors can assess the integrity and function of the vagus nerve.
In some cases, imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be ordered. These imaging tests can provide detailed images of the structures surrounding the vagus nerve, allowing doctors to identify any abnormalities or sources of compression.
Specialized tests may also be used to diagnose specific vagus nerve disorders. For example, if a patient is suspected to have vocal cord dysfunction related to vagus nerve dysfunction, a laryngoscopy may be performed. This test involves inserting a small camera into the throat to visualize the vocal cords and assess their movement.
Overall, the diagnostic process for vagus nerve disorders involves a comprehensive evaluation of the patient’s symptoms, medical history, and physical examination. Through the use of various diagnostic tests, doctors can accurately diagnose and assess the severity of vagus nerve disorders, leading to appropriate treatment decisions.
Treatment Options for Vagus Nerve Disorders
Treatment for vagus nerve disorders depends on the specific condition and its underlying cause. In many cases, a multidisciplinary approach involving different specialists may be necessary to address the diverse symptoms and needs of the patient.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It plays a crucial role in regulating various bodily functions, including heart rate, digestion, and breathing. When the vagus nerve is disrupted or damaged, it can lead to a wide range of symptoms and complications.
Medication and Non-Surgical Treatments
For certain vagus nerve disorders, medication can help manage symptoms and improve quality of life. Medications may include pain relievers, anti-seizure drugs, anti-nausea medications, and muscle relaxants. These medications target specific symptoms and aim to restore normal functioning of the vagus nerve.
In addition to medication, non-surgical treatments such as physical therapy, speech therapy, and biofeedback may also be recommended to address specific symptoms and promote recovery. Physical therapy can help improve muscle strength and coordination, while speech therapy can assist with speech and swallowing difficulties. Biofeedback, on the other hand, utilizes electronic devices to monitor and provide feedback on bodily functions, helping patients gain control over their physiological responses.
Surgical Interventions for Vagus Nerve Disorders
In severe cases or when conservative methods fail to provide relief, surgical interventions may be necessary. Surgical options for vagus nerve disorders can include nerve decompression surgery, nerve grafting, or vagus nerve stimulation.
Nerve decompression surgery involves relieving pressure on the vagus nerve by removing any surrounding structures that may be compressing it. This procedure aims to restore normal nerve function and alleviate symptoms such as pain and numbness.
Nerve grafting, on the other hand, involves replacing a damaged section of the vagus nerve with a healthy nerve graft. This technique allows for the regeneration of nerve fibers and can help restore normal nerve function over time.
Vagus nerve stimulation (VNS) is a procedure that involves implanting a device in the chest wall that delivers electrical impulses to the vagus nerve. These electrical impulses help regulate nerve activity and can reduce the frequency and severity of symptoms associated with vagus nerve disorders.
It is important to note that surgical interventions carry their own risks and potential complications. Therefore, these options are typically considered when other treatments have been unsuccessful or when the condition is significantly impacting the patient’s quality of life.
In conclusion, treatment options for vagus nerve disorders vary depending on the specific condition and its underlying cause. Medication and non-surgical treatments can help manage symptoms, while surgical interventions may be necessary for severe cases. It is essential for patients to work closely with their healthcare team to determine the most appropriate treatment plan for their individual needs.
The Importance of Follow-Up Care
Following the initial diagnosis and treatment of vagus nerve disorders, ongoing follow-up care is crucial to monitor progress and make necessary adjustments to the treatment plan.
Monitoring Progress and Adjusting Treatment
Regular check-ups allow doctors to assess the effectiveness of the chosen treatment approach and make any necessary modifications. This may involve changes in medication dosage, the addition of new therapies, or adjustments to surgical interventions based on the patient’s response and overall health status.
Long-Term Management of Vagus Nerve Disorders
Vagus nerve disorders often require long-term management to address chronic symptoms and prevent complications. Patient education and self-management strategies are essential for coping with the condition effectively. This may involve lifestyle modifications, dietary changes, stress management techniques, and ongoing rehabilitation therapies.
In Conclusion
When seeking care for vagus nerve disorders, it is crucial to consult the appropriate medical professionals. Neurologists, otolaryngologists, and gastroenterologists have the knowledge and expertise necessary to diagnose, treat, and manage these conditions effectively. Through a comprehensive diagnostic process, various treatment options, and ongoing follow-up care, individuals with vagus nerve disorders can aim to improve their quality of life and overall well-being.