The human body is a complex network of interconnected systems, each playing a crucial role in maintaining our overall health and well-being. One such system is the vagus nerve, a powerful bundle of nerves that stretches from the brainstem to the abdomen. The vagus nerve, also known as the tenth cranial nerve, is an essential component of the parasympathetic nervous system, responsible for regulating various bodily functions, including digestion, heart rate, and even mood.
An Overview of the Vagus Nerve
The vagus nerve is a vital part of the autonomic nervous system, which controls involuntary bodily functions. It is the longest cranial nerve and is divided into two branches: the sensory and motor branches. The sensory branch gathers information from various organs and sends it back to the brain, while the motor branch carries instructions from the brain to the organs, signaling them to perform specific actions.
The vagus nerve, also known as the “wandering nerve,” gets its name from its extensive distribution throughout the body. It meanders through various organs, connecting them to the brain and facilitating communication between them. This intricate network of fibers allows for the seamless coordination of essential bodily functions.
The Role and Function of the Vagus Nerve
The vagus nerve plays a crucial role in maintaining homeostasis within the body. It regulates heart rate, breathing, digestion, and other functions necessary for our survival. Without the vagus nerve, our bodies would struggle to maintain a stable internal environment.
One of the key functions of the vagus nerve is its involvement in the body’s stress response system. When we encounter a stressful situation, the vagus nerve helps to activate the “rest and digest” response, counteracting the “fight or flight” response. This activation helps to reduce anxiety, promote relaxation, and restore balance within the body.
Moreover, the vagus nerve is responsible for the complex process of digestion. It stimulates the secretion of gastric juices and enzymes necessary for breaking down food and absorbing nutrients. Without the vagus nerve’s influence, our digestive system would struggle to efficiently process the food we consume.
In addition to its role in digestion, the vagus nerve also controls the contraction of smooth muscles throughout the body. This includes the smooth muscles in the walls of our digestive tract, allowing food to move through the system smoothly. Without the vagus nerve’s regulation, we would experience difficulties in the movement of food, leading to digestive issues.
Anatomy of the Vagus Nerve
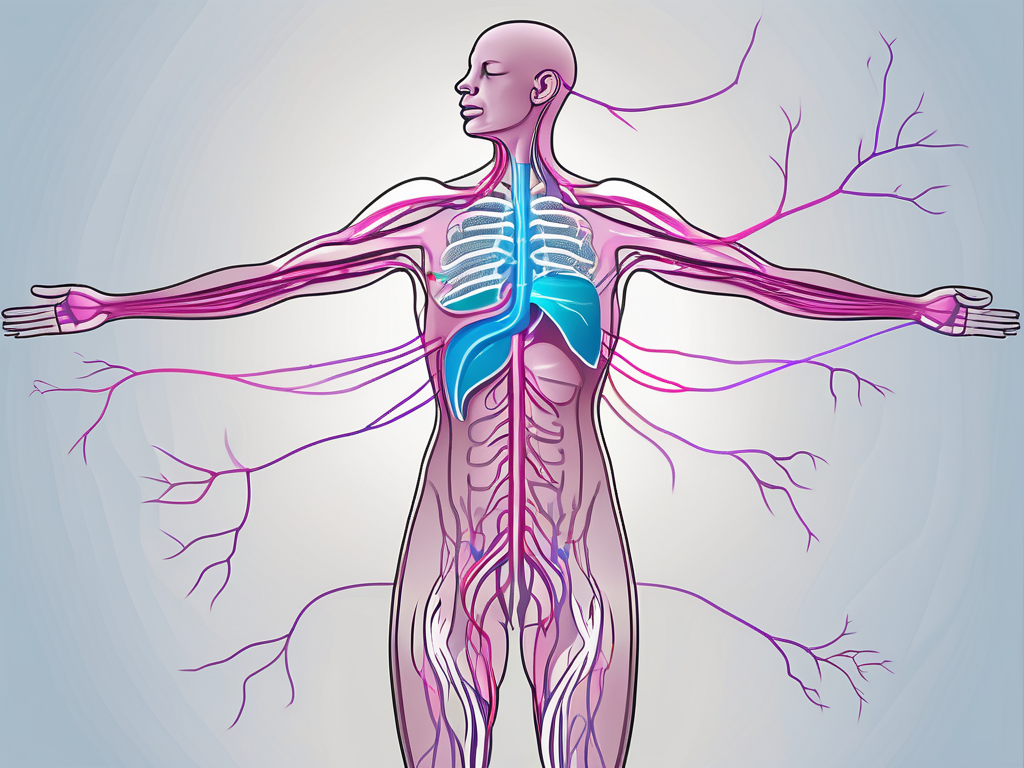
The vagus nerve consists of thousands of small fibers, with both sensory and motor components. It originates in the medulla oblongata, a part of the brainstem located at the base of the skull. From there, it descends through the neck and chest, branching out to various organs along its path.
As the vagus nerve extends its reach, it forms connections with organs such as the heart, lungs, stomach, liver, and intestines. These connections allow for efficient communication and coordination between the brain and the body. It is through these intricate pathways that the vagus nerve carries out its essential functions.
Furthermore, the vagus nerve’s extensive distribution throughout the body highlights its significance in maintaining overall health and well-being. Its far-reaching connections enable it to monitor and regulate various bodily functions, ensuring that everything is working in harmony.
In conclusion, the vagus nerve is a remarkable component of the autonomic nervous system. Its role in maintaining homeostasis, regulating digestion, and facilitating the body’s stress response system cannot be overstated. Understanding the anatomy and functions of the vagus nerve provides valuable insights into the intricate workings of our bodies.
Common Disorders of the Vagus Nerve
While the vagus nerve is vital for our well-being, it is not exempt from potential disorders that can significantly impact our health. Several conditions can affect the proper functioning of the vagus nerve, leading to various symptoms and complications.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It extends from the brainstem to various organs in the neck, chest, and abdomen, playing a crucial role in regulating many bodily functions, including digestion, heart rate, and breathing.
Gastroparesis: A Digestive Disorder
Gastroparesis is a condition characterized by delayed stomach emptying. This disorder occurs when the vagus nerve is damaged or dysfunctional, leading to impaired movement of food through the digestive tract. The vagus nerve normally sends signals to the stomach muscles, instructing them to contract and push food into the small intestine. However, when the vagus nerve is not functioning properly, the stomach muscles may not receive these signals, causing food to remain in the stomach for longer periods.
Individuals with gastroparesis may experience a range of symptoms, including nausea, vomiting, bloating, and a feeling of fullness even after eating a small amount. These symptoms can significantly impact a person’s quality of life, making it difficult to maintain a regular eating schedule and leading to nutritional deficiencies. Treatment for gastroparesis often involves dietary modifications, such as eating smaller, more frequent meals, and avoiding foods that are difficult to digest. In some cases, medication management or surgical interventions may be necessary to improve gastric motility.
Vasovagal Syncope: A Circulatory Disorder
Vasovagal syncope, also known as fainting, is a common condition associated with an abnormal vagus nerve response. This disorder occurs when the brain fails to receive adequate blood flow due to a sudden drop in heart rate and blood pressure. The vagus nerve plays a crucial role in regulating heart rate and blood pressure, so any dysfunction in this nerve can lead to episodes of fainting.
Individuals with vasovagal syncope may experience symptoms such as dizziness, lightheadedness, and loss of consciousness. These episodes are often triggered by specific stimuli, such as prolonged standing, emotional stress, or the sight of blood. While vasovagal syncope is typically harmless and resolves on its own, it can be unsettling and may require medical evaluation to rule out other underlying causes.
Vagus Nerve Stimulation and Epilepsy
In recent years, vagus nerve stimulation (VNS) has emerged as a potential treatment for epilepsy, a neurological disorder characterized by recurrent seizures. VNS involves the implantation of a device that stimulates the vagus nerve through electrical impulses, helping to reduce the frequency and severity of seizures.
The exact mechanism of how VNS works in treating epilepsy is not fully understood. However, it is believed that the electrical stimulation of the vagus nerve alters the abnormal brain activity that leads to seizures. VNS is typically used as an adjunctive therapy for individuals with epilepsy whose seizures are not well-controlled with medications alone.
While VNS does not cure epilepsy, it offers hope for individuals who have not found adequate seizure control through other treatment options. The procedure to implant the VNS device is generally safe and well-tolerated, with potential side effects including hoarseness, cough, and shortness of breath. Regular follow-up visits with healthcare professionals are necessary to monitor the effectiveness of VNS and adjust the stimulation settings as needed.
Symptoms and Diagnosis of Vagus Nerve Disorders
Recognizing the symptoms of vagus nerve disorders is vital for prompt diagnosis and appropriate management. While symptoms can vary depending on the specific condition and individual, there are common indicators that can alert healthcare professionals to a potential vagus nerve dysfunction.
Recognizing the Symptoms
For disorders such as gastroparesis, symptoms may include persistent nausea, vomiting, early satiety, and abdominal bloating. These symptoms can significantly impact an individual’s quality of life, making it difficult to enjoy meals or maintain a healthy weight. In severe cases, malnutrition and dehydration may occur, requiring medical intervention.
Individuals with vasovagal syncope may experience sudden fainting episodes, preceded by lightheadedness and palpitations. These episodes can be frightening and may lead to injuries if they occur in dangerous situations, such as while driving or operating heavy machinery. It is crucial for individuals with vasovagal syncope to be aware of their triggers and take necessary precautions to prevent accidents.
In the case of epilepsy, recurrent seizures that are resistant to medication can indicate the need for further evaluation, potentially leading to the consideration of VNS therapy. Epilepsy can significantly impact an individual’s daily life, affecting their ability to work, drive, or engage in activities that may trigger seizures. Proper diagnosis and treatment are essential to help individuals with epilepsy manage their condition and improve their overall well-being.
Diagnostic Procedures and Tests
Diagnosing vagus nerve disorders typically involves a comprehensive evaluation that may include a combination of medical history review, physical examination, and specialized tests. These tests can range from simple bloodwork and imaging studies to more invasive procedures, such as endoscopy or electroencephalography (EEG).
During a medical history review, healthcare professionals will ask detailed questions about the individual’s symptoms, their duration, and any potential triggers or underlying medical conditions. This information helps in narrowing down the possible causes and guiding further diagnostic steps.
A physical examination may involve assessing the individual’s vital signs, performing neurological tests, and examining specific body areas related to the suspected vagus nerve disorder. For example, in the case of gastroparesis, a healthcare professional may perform an abdominal examination to check for signs of bloating or tenderness.
Specialized tests, such as gastric emptying studies, can provide valuable information about the functioning of the vagus nerve and its impact on the digestive system. These tests involve tracking the movement of food through the stomach and can help confirm a diagnosis of gastroparesis.
Electroencephalography (EEG) is a non-invasive test that measures the electrical activity of the brain. It is commonly used to diagnose and monitor epilepsy. During an EEG, small electrodes are attached to the scalp, and the individual’s brain activity is recorded. This test can help identify abnormal brain wave patterns that are characteristic of epilepsy and guide treatment decisions.
In some cases, additional imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be necessary to visualize the structures surrounding the vagus nerve and identify any abnormalities.
The goal of these diagnostic procedures and tests is to identify the underlying cause of the symptoms and determine the most appropriate treatment approach. Early and accurate diagnosis is crucial for effective management of vagus nerve disorders and improving the quality of life for individuals affected by these conditions.
Treatment Options for Vagus Nerve Disorders
When it comes to treating vagus nerve disorders, a multi-faceted approach is often necessary to address the unique needs and circumstances of each individual. Treatment options may include medication management, various therapies, and, in some cases, surgical interventions.
Medications and Therapies
In the management of vagus nerve disorders, medications are commonly prescribed to alleviate symptoms and promote normal bodily functions. For gastroparesis, prokinetic agents may be prescribed to assist in improving gastric motility. In the case of epilepsy, antiepileptic drugs are often prescribed to reduce the frequency and severity of seizures. Additionally, therapies such as physical therapy, occupational therapy, and biofeedback can be beneficial in improving overall well-being.
Surgical Interventions
For individuals who do not respond well to medications or therapies, surgical interventions may be considered. In cases of severe gastroparesis, gastric electrical stimulation or surgical procedures to bypass the vagus nerve can restore normal digestive function. Likewise, for epilepsy patients who do not achieve seizure control with medications alone, VNS may be recommended as a surgical treatment option.
The Impact of Vagus Nerve Disorders on Quality of Life
Vagus nerve disorders can significantly impact a person’s quality of life, affecting both their physical and mental well-being. Understanding the potential implications of these disorders is essential for comprehensive management and support.
Physical Health Implications
Vagus nerve disorders, such as gastroparesis or syncope, can lead to disruptions in daily activities, affecting an individual’s ability to eat, work, or engage in social interactions. The physical symptoms associated with these disorders can be distressing, leading to discomfort and reduced productivity. Timely diagnosis and appropriate treatment can help alleviate these challenges, restoring a person’s physical well-being.
Mental Health Implications
The impact of vagus nerve disorders extends beyond physical health, often affecting an individual’s mental well-being. Chronic conditions such as gastroparesis or epilepsy can contribute to feelings of frustration, anxiety, and depression. The unpredictability of symptoms or the side effects of medications can further exacerbate these emotional challenges. A holistic approach to treatment, including psychological support and counseling, can help individuals cope with the emotional toll of living with a vagus nerve disorder.
In conclusion, understanding disorders involving the vagus nerve is vital for both healthcare professionals and individuals affected by these conditions. By delving into the anatomy, function, and common disorders of the vagus nerve, we can gain insights into the complex interplay between the nervous system and overall well-being. With early recognition, accurate diagnosis, and appropriate treatment, individuals affected by vagus nerve disorders can improve their quality of life and regain control over their health.