Gastrointestinal disorders can have a significant impact on individuals’ quality of life, causing discomfort, pain, and disruption in daily activities. Consequently, understanding the underlying mechanisms that contribute to these disorders is crucial for developing effective treatment and prevention strategies. In recent years, research has increasingly focused on exploring the link between the vagus nerve and gastrointestinal disorders, shedding light on the intricate connection between the nervous system and the digestive system.
An Overview of the Vagus Nerve
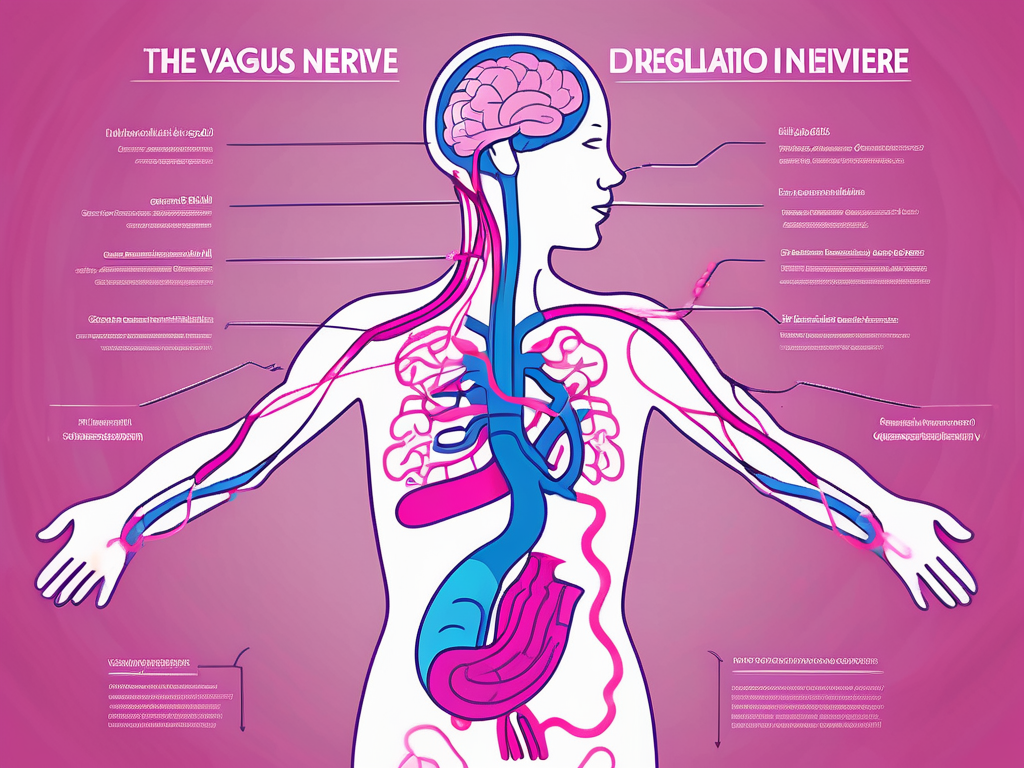
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex nerve in the human body. It originates in the brainstem and branches out to various organs, including the heart, lungs, liver, and gastrointestinal tract. The vagus nerve plays a crucial role in regulating many essential bodily functions, such as heart rate, breathing, digestion, and immune response.
The Anatomy and Function of the Vagus Nerve
The vagus nerve consists of sensory and motor fibers that transmit signals between the brain and the organs it innervates. Sensory fibers carry information from the organs to the brain, while motor fibers transmit signals from the brain to the organs, regulating their functions. This bidirectional communication enables the vagus nerve to coordinate complex physiological processes and maintain homeostasis.
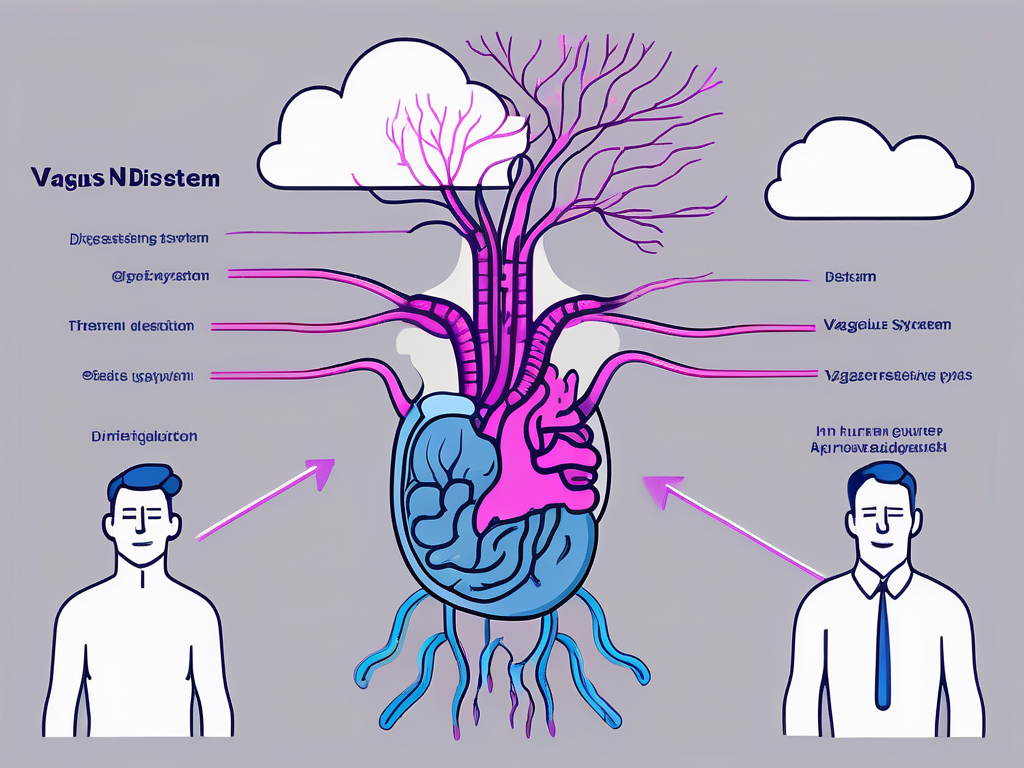
One of the essential functions of the vagus nerve is its role in the body’s autonomic nervous system. The autonomic nervous system is responsible for controlling involuntary bodily functions, such as heart rate, blood pressure, and digestion. The vagus nerve, as the main parasympathetic branch of the autonomic nervous system, predominantly regulates rest-and-digest responses, promoting relaxation, digestion, and nutrient absorption.
Let’s delve deeper into the anatomy of the vagus nerve. It emerges from the medulla oblongata, the lower part of the brainstem, and descends through the neck, chest, and abdomen, making connections with various organs along the way. The vagus nerve is divided into two main branches: the cranial and the spinal branches.
The cranial branches of the vagus nerve are responsible for innervating organs in the head and neck region. These branches supply the muscles involved in swallowing, speaking, and facial expressions. They also provide sensory information from the throat, larynx, and ears, allowing us to experience sensations like taste, sound, and touch.
The spinal branches of the vagus nerve, on the other hand, extend down to the thoracic and abdominal regions. These branches innervate organs such as the heart, lungs, liver, and gastrointestinal tract. By regulating the functions of these organs, the vagus nerve ensures the proper functioning of vital processes like breathing, digestion, and metabolism.
Furthermore, the vagus nerve is not just involved in physical functions but also has a significant impact on our mental and emotional well-being. It is intricately connected to the brain’s limbic system, which controls emotions, memory, and behavior. This connection allows the vagus nerve to influence our mood, stress response, and overall mental health.
Research has shown that stimulating the vagus nerve can have therapeutic effects on various conditions. Vagus nerve stimulation (VNS) is a treatment method that involves delivering electrical impulses to the nerve, helping to alleviate symptoms of epilepsy, depression, and even inflammatory diseases. This highlights the potential of the vagus nerve as a target for medical interventions and the ongoing exploration of its therapeutic applications.
In conclusion, the vagus nerve is a remarkable component of the human body’s intricate nervous system. Its extensive reach and multifaceted functions make it a vital player in maintaining our overall health and well-being. Understanding the anatomy and function of the vagus nerve opens up new avenues for medical advancements and potential treatments for a wide range of conditions.
The Connection Between the Vagus Nerve and the Digestive System
The intricate connection between the vagus nerve and the digestive system has garnered increasing attention in recent years. The vagus nerve exerts profound influence over various aspects of digestive health, including gut motility, secretion, and immune function.
How the Vagus Nerve Influences Digestive Health
The vagus nerve modulates the muscles’ contractions in the digestive tract, known as gut motility, helping to propel food and waste products through the gastrointestinal system. When the vagus nerve is functioning correctly, it promotes efficient digestion and prevents issues such as constipation or diarrhea.
But the influence of the vagus nerve on the digestive system goes beyond just gut motility. It also plays a crucial role in regulating the secretion of digestive enzymes and hormones necessary for proper digestion. These enzymes and hormones are responsible for breaking down food into smaller molecules that can be absorbed by the body. Dysfunction of the vagus nerve can disrupt these processes, leading to digestive disorders such as bloating, indigestion, or malabsorption.
Furthermore, the vagus nerve is involved in the communication between the gut and the brain, forming what is known as the gut-brain axis. This bidirectional communication allows the brain to receive information from the gut and vice versa. The vagus nerve acts as a messenger, relaying signals between the two, influencing not only digestive function but also mood, appetite, and overall well-being.
Research has also shown that the vagus nerve has a significant impact on the immune system within the digestive system. It helps regulate the release of immune cells and cytokines, which are essential for maintaining a healthy gut environment. Dysfunction of the vagus nerve can disrupt this delicate balance, leading to inflammation and increased susceptibility to gastrointestinal infections.
Moreover, studies have suggested that the vagus nerve may play a role in the gut’s microbial composition, known as the gut microbiota. The gut microbiota consists of trillions of microorganisms that reside in the digestive system and play a crucial role in various aspects of health, including digestion, metabolism, and immune function. The vagus nerve may influence the composition and diversity of the gut microbiota, further highlighting its importance in digestive health.
Understanding the connection between the vagus nerve and the digestive system opens up new possibilities for therapeutic interventions. Researchers are exploring techniques such as vagus nerve stimulation to treat various digestive disorders, including inflammatory bowel disease, gastroparesis, and irritable bowel syndrome.
In conclusion, the vagus nerve plays a vital role in maintaining digestive health. Its influence extends beyond gut motility and encompasses the regulation of digestive enzymes, immune function, gut-brain communication, and gut microbiota. Further research in this field will undoubtedly shed more light on the intricate relationship between the vagus nerve and the digestive system, paving the way for innovative treatments and interventions.
Common Gastrointestinal Disorders Linked to Vagus Nerve Dysfunction
Vagus nerve dysfunction has been implicated in various gastrointestinal disorders, highlighting its significance in maintaining digestive health. The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system, responsible for regulating many vital functions in the body, including digestion.
When the vagus nerve’s normal functioning is compromised, it can have a profound impact on gastrointestinal health, leading to the development of several disorders. Two such disorders that have been extensively studied in relation to vagus nerve dysfunction are gastroparesis and gastroesophageal reflux disease (GERD).
Gastroparesis and the Vagus Nerve
Gastroparesis is a condition characterized by delayed gastric emptying, where the stomach fails to contract and empty food properly. Research suggests that vagus nerve damage or impairment is a common underlying cause of gastroparesis. The vagus nerve plays a crucial role in coordinating the muscle contractions of the stomach, which are necessary for propelling food through the digestive tract.
When the vagus nerve’s motor function is compromised, it can disrupt the coordinated muscle contractions needed for proper stomach emptying, leading to symptoms such as nausea, vomiting, and abdominal pain. Furthermore, the vagus nerve also plays a role in signaling the release of digestive enzymes and stomach acid, further contributing to the impaired digestive function seen in gastroparesis.
Understanding the connection between vagus nerve dysfunction and gastroparesis has opened up new avenues for potential treatment options. Researchers are exploring various approaches, including vagus nerve stimulation, to restore normal gastric motility and alleviate symptoms in individuals with gastroparesis.
Gastroesophageal Reflux Disease (GERD) and the Vagus Nerve
Gastroesophageal Reflux Disease (GERD) is a chronic condition characterized by the backward flow of stomach acid into the esophagus, causing heartburn, chest pain, and regurgitation. While the primary cause of GERD is the malfunctioning of the lower esophageal sphincter (LES), studies have indicated that alterations in vagal tone may contribute to GERD development.
The vagus nerve plays a crucial role in regulating the lower esophageal sphincter, a muscular valve that prevents stomach acid from refluxing into the esophagus. Dysfunction in the vagus nerve’s regulation of this sphincter can lead to its improper functioning, increasing the risk of acid reflux. Additionally, the vagus nerve also influences the secretion of mucus in the esophagus, which helps protect it from the corrosive effects of stomach acid.
Understanding the role of the vagus nerve in GERD has led to the exploration of novel treatment approaches. Vagus nerve stimulation, a technique that involves the use of electrical impulses to modulate the nerve’s activity, has shown promise in managing GERD symptoms in some individuals. By restoring normal vagal tone and improving LES function, vagus nerve stimulation may offer a potential therapeutic option for those with GERD.
In conclusion, the vagus nerve plays a critical role in maintaining proper gastrointestinal function. Dysfunction or damage to this important nerve can lead to the development of various gastrointestinal disorders, including gastroparesis and GERD. Understanding the intricate relationship between the vagus nerve and these disorders opens up new possibilities for targeted treatments and interventions, offering hope for improved digestive health and overall well-being.
Understanding Vagus Nerve Stimulation Therapy
Vagus Nerve Stimulation (VNS) therapy is an emerging treatment modality that aims to harness the regulatory potential of the vagus nerve to manage various health conditions, including gastrointestinal disorders.
The Process and Purpose of Vagus Nerve Stimulation
VNS therapy involves the surgical implantation of a device that delivers electrical impulses to the vagus nerve. By modulating the vagus nerve’s activity, VNS therapy aims to restore proper nerve function and regulate autonomic processes associated with gastrointestinal disorders. It has shown promise in managing conditions such as gastroparesis and epilepsy. However, further research is needed to fully understand its potential benefits and long-term effects.
The Potential of Vagus Nerve Stimulation in Treating Gastrointestinal Disorders
Preliminary studies suggest that VNS therapy may offer a novel approach to treating gastrointestinal disorders that are resistant to traditional therapies. By targeting the vagus nerve, it may help regulate gut motility, secretion, and immune response, offering a more comprehensive treatment option for individuals with chronic digestive issues. Ongoing research is exploring the efficacy and safety of VNS therapy, providing hope for improved management of gastrointestinal disorders in the future.
The Future of Vagus Nerve Research in Gastroenterology
As the link between the vagus nerve and gastrointestinal disorders continues to unfold, the future holds great promise in improving our understanding and management of these conditions.
Emerging Studies on the Vagus Nerve and Gut Health
Researchers are actively investigating the complex interplay between the vagus nerve, the gut microbiota, and overall gut health. Studies suggest that the vagus nerve may play a role in mediating the communication between the gut and the brain, influencing not only digestive function but also mental health and well-being. Understanding these interactions could pave the way for tailored interventions that target both the gut and nervous system for improved gastrointestinal health.
Potential Implications for Treatment and Prevention Strategies
The evolving field of vagus nerve research in gastroenterology holds potential implications for developing innovative treatment and prevention strategies for gastrointestinal disorders. By uncovering the mechanisms underlying vagus nerve dysfunction in these conditions, researchers can identify novel therapeutic targets and explore non-invasive interventions that modulate vagal activity. This may open doors for personalized healthcare approaches tailored to individual needs, ultimately improving patient outcomes in the realm of digestive health.
In conclusion, the link between the vagus nerve and gastrointestinal disorders underscores the complex interplay between the nervous system and the digestive system. Understanding the role of the vagus nerve in maintaining digestive health provides valuable insights that can inform the development of novel treatment approaches for individuals with gastrointestinal disorders. As research continues to unravel the mysteries surrounding the vagus nerve, the future holds promising possibilities for improved understanding, management, and prevention of gastroenterological conditions.