In recent years, there has been growing interest in the complex interplay between neurological disorders and gastrointestinal conditions. One particular connection that has garnered attention is the link between vagus nerve disorders and small intestinal bacterial overgrowth (SIBO). The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including digestion and immune response. Understanding this connection is essential for developing effective strategies in the diagnosis and treatment of individuals affected by both disorders.
Exploring the Vagus Nerve: An Overview
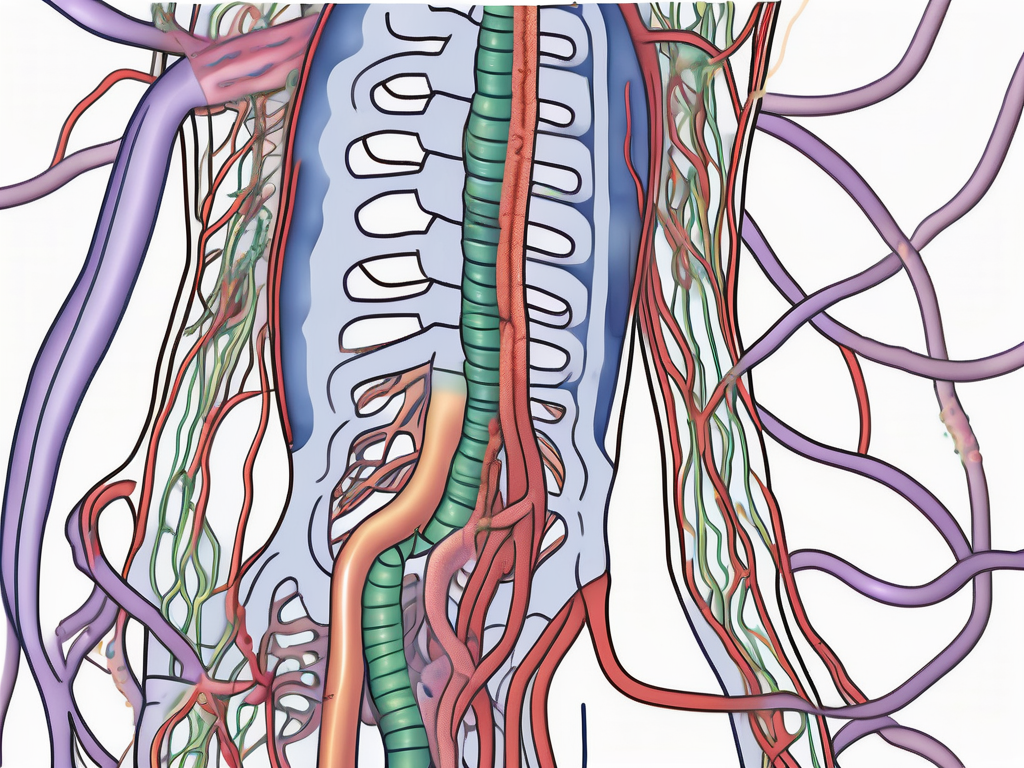
To comprehend the link between vagus nerve disorders and SIBO, it is imperative to examine the vagus nerve’s role and function within the human body. The vagus nerve, originating in the brainstem and extending down to the abdomen, serves as a critical communication channel between the central nervous system and the gastrointestinal system. It is responsible for transmitting sensory and motor signals, playing a vital role in regulating digestion, gut motility, and the gut-brain axis.
The Role and Function of the Vagus Nerve
The vagus nerve is primarily responsible for aiding in digestion by activating the parasympathetic nervous system, also known as the “rest and digest” response. When functioning optimally, the vagus nerve stimulates gastric acid secretion, promotes gastrointestinal motility, and regulates the release of pancreatic enzymes and bile. This intricate network of signals ensures that the digestive system operates smoothly and efficiently.
Furthermore, the vagus nerve plays a crucial role in the gut-brain axis, a bidirectional communication system between the gut and the brain. Through this axis, the vagus nerve transmits information about the gut’s state to the brain, influencing mood, appetite, and overall well-being. It also facilitates the release of neurotransmitters, such as serotonin, which plays a significant role in regulating emotions and mood.
Common Disorders Associated with the Vagus Nerve
Several disorders can affect the vagus nerve, compromising its ability to regulate gastrointestinal function adequately. One such disorder is gastroparesis, a condition characterized by delayed gastric emptying. When the vagus nerve is damaged or dysfunctional, the stomach muscles may not receive the necessary signals to contract and push food into the small intestine, leading to symptoms such as bloating, nausea, and vomiting.
Gastroesophageal reflux disease (GERD) is another disorder closely associated with vagus nerve dysfunction. The vagus nerve helps regulate the lower esophageal sphincter, a ring of muscles that prevents stomach acid from flowing back into the esophagus. If the vagus nerve is impaired, the lower esophageal sphincter may not function properly, resulting in acid reflux, heartburn, and discomfort.
Chronic inflammation of the digestive tract, such as in conditions like Crohn’s disease or ulcerative colitis, can also impact the vagus nerve. Inflammation can disrupt the normal functioning of the nerve, leading to altered gastrointestinal motility, pain, and other digestive symptoms.
It is important to note that vagus nerve disorders can have far-reaching effects beyond the digestive system. The vagus nerve is intricately connected to various other bodily functions, including heart rate regulation, immune response modulation, and stress management. Therefore, addressing vagus nerve dysfunction is crucial not only for digestive health but for overall well-being.
Delving into SIBO: A Closer Look
SIBO, short for Small Intestinal Bacterial Overgrowth, is a condition that affects the small intestine. It occurs when there is an excessive growth of bacteria in this part of the digestive system. Normally, the small intestine maintains a relatively low bacterial population, allowing for proper nutrient absorption. However, when the delicate balance between the gut microbiota and the immune system is disrupted, an accumulation of bacteria occurs, leading to gastrointestinal symptoms and inflammation.
The causes of SIBO can vary, but it is typically associated with impaired gut motility, structural abnormalities in the gastrointestinal tract, or an underlying gastrointestinal condition. These conditions can include irritable bowel syndrome (IBS), Crohn’s disease, celiac disease, and gastrointestinal surgeries. When these factors are present, the risk of developing SIBO increases.
Understanding SIBO: Causes and Symptoms
Impaired gut motility refers to a condition where the muscles in the digestive system do not contract properly, leading to a slowdown in the movement of food through the intestines. This can create an environment where bacteria can thrive and multiply. Structural abnormalities in the gastrointestinal tract, such as strictures or diverticula, can also contribute to the development of SIBO by disrupting the normal flow of food and allowing bacteria to accumulate.
Individuals with underlying gastrointestinal conditions may be more susceptible to SIBO. For example, individuals with irritable bowel syndrome (IBS) often experience symptoms such as abdominal pain, bloating, and changes in bowel habits. These symptoms can be exacerbated by the presence of SIBO, further impacting an individual’s quality of life.
The Impact of SIBO on Digestive Health
Untreated SIBO can have far-reaching effects on digestive health. The overgrowth of bacteria in the small intestine can interfere with nutrient absorption, leading to malnutrition and deficiencies in vital vitamins and minerals. This can result in a range of symptoms, including fatigue, weakness, and even neurological problems.
Moreover, the accumulation of bacteria can trigger an immune response, causing chronic inflammation in the gut and exacerbating existing gastrointestinal conditions. Inflammation can further damage the lining of the small intestine, impairing its ability to absorb nutrients effectively. This vicious cycle can lead to a decline in overall health and well-being.
Recognizing and addressing the link between vagus nerve disorders and SIBO is imperative for optimal patient management. The vagus nerve plays a crucial role in regulating the movement of food through the digestive system. When this nerve is compromised, it can disrupt gut motility and contribute to the development of SIBO.
In conclusion, SIBO is a complex condition that can have a significant impact on digestive health. Understanding the causes and symptoms of SIBO is essential for early detection and effective management. By addressing the underlying factors contributing to SIBO and implementing appropriate treatment strategies, individuals can improve their quality of life and restore balance to their digestive system.
The Connection between Vagus Nerve Disorders and SIBO
The complex relationship between vagus nerve disorders and Small Intestinal Bacterial Overgrowth (SIBO) is multifaceted and warrants detailed exploration. Emerging evidence suggests that vagus nerve dysfunction can contribute to the development and perpetuation of SIBO, while the presence of SIBO can also impact vagus nerve function, creating a vicious cycle.
How Vagus Nerve Disorders Can Lead to SIBO
Individuals with vagus nerve disorders may experience impaired gastrointestinal motility, characterized by the slow movement of food through the digestive tract. This stasis creates a favorable environment for bacterial overgrowth in the small intestine. The vagus nerve, a major component of the parasympathetic nervous system, plays a crucial role in regulating various digestive functions, including the migrating motor complex (MMC).
The MMC is a series of contractions that help prevent bacterial buildup in the small intestine. Dysfunction in the vagus nerve can disrupt the MMC, leading to SIBO. When the MMC fails to function properly, it allows bacteria to accumulate and thrive in the small intestine, leading to an overgrowth that can cause a range of symptoms such as bloating, abdominal pain, and diarrhea.
The Interplay of Neurological and Digestive Health
Furthermore, neurological conditions such as Parkinson’s disease, multiple sclerosis, and autonomic neuropathy can compromise vagus nerve function, further increasing the risk of SIBO. In Parkinson’s disease, for example, degeneration of the dopaminergic neurons in the brain can lead to vagus nerve dysfunction, impairing the proper regulation of gastrointestinal motility and increasing the likelihood of SIBO.
Conversely, the presence of SIBO can induce an immune response and inflammation, which can lead to nerve damage and dysfunction, thus perpetuating the cycle of vagus nerve disorders and SIBO. The immune response triggered by the overgrowth of bacteria in the small intestine can cause damage to the vagus nerve, exacerbating its dysfunction and further impairing gastrointestinal motility.
Moreover, chronic inflammation resulting from SIBO can lead to the release of pro-inflammatory cytokines, which can affect the integrity of the blood-brain barrier. This compromised barrier can allow harmful substances to enter the brain, potentially contributing to the development or progression of neurological disorders.
Understanding the intricate relationship between vagus nerve disorders and SIBO is crucial for developing effective treatment strategies. Targeting both the underlying vagus nerve dysfunction and the bacterial overgrowth in the small intestine is essential for breaking the cycle and improving overall gastrointestinal health.
Diagnosis and Treatment Options
A key challenge in managing individuals with both vagus nerve disorders and SIBO lies in effectively diagnosing and treating the conditions. Accurate diagnosis is essential to tailor appropriate treatment strategies and improve patient outcomes.
When it comes to diagnosing vagus nerve disorders, healthcare professionals often embark on a comprehensive assessment of symptoms. This involves carefully evaluating the patient’s medical history and conducting a thorough physical examination. However, to obtain a more precise diagnosis, specialized tests such as gastric emptying studies and electrogastrography may be employed. These tests provide valuable insights into the functioning of the vagus nerve and help determine the extent of the disorder.
On the other hand, detecting SIBO typically requires a different approach. A breath test is commonly used to measure the presence of specific gases produced by bacterial metabolism. By analyzing the levels of these gases, healthcare professionals can identify the presence of bacterial overgrowth in the small intestine, which is a hallmark of SIBO. This diagnostic tool, combined with the aforementioned medical history and physical examination, helps healthcare professionals identify and characterize the relationship between vagus nerve disorders and SIBO.
Identifying Vagus Nerve Disorders and SIBO
Diagnosing vagus nerve disorders often involves a comprehensive assessment of symptoms, along with specialized tests such as gastric emptying studies and electrogastrography. Detecting SIBO typically requires a breath test to measure the presence of specific gases produced by bacterial metabolism. These diagnostic tools, combined with a thorough medical history and physical examination, help healthcare professionals identify and characterize the relationship between vagus nerve disorders and SIBO.
Moreover, it is important to note that the symptoms of vagus nerve disorders and SIBO can often overlap, making the diagnosis even more challenging. Symptoms such as abdominal pain, bloating, and altered bowel movements can be present in both conditions. Therefore, healthcare professionals must carefully analyze the clinical presentation and rely on diagnostic tests to differentiate between the two.
Additionally, it is worth mentioning that the relationship between vagus nerve disorders and SIBO is complex and multifaceted. While SIBO can be a consequence of impaired vagus nerve function, it can also exacerbate the symptoms of vagus nerve disorders. This intricate interplay necessitates a comprehensive diagnostic approach to accurately identify and address both conditions.
Modern Approaches to Treatment and Management
Treatment strategies for individuals affected by both vagus nerve disorders and SIBO often involve a multidisciplinary approach. This means that healthcare professionals from various specialties collaborate to develop a comprehensive treatment plan tailored to the patient’s unique needs.
One of the primary treatment approaches for individuals with vagus nerve disorders and SIBO is dietary modification. A low fermentable oligosaccharide, disaccharide, monosaccharide, and polyols (FODMAP) diet is commonly recommended to alleviate symptoms and reduce bacterial overgrowth. This diet restricts the consumption of certain carbohydrates that are known to ferment in the gut and contribute to bacterial proliferation. By adhering to a FODMAP diet, patients can often experience a reduction in symptoms and an improvement in overall gut health.
In addition to dietary modifications, prokinetic medications may be prescribed to enhance gut motility and prevent stasis. These medications work by stimulating the muscles of the gastrointestinal tract, facilitating the movement of food and waste through the digestive system. By improving gut motility, prokinetic medications can help prevent the accumulation of bacteria in the small intestine, thereby reducing the risk of SIBO.
Furthermore, managing the psychological aspects of vagus nerve disorders and their impact on SIBO is crucial. Cognitive-behavioral therapy and stress management techniques can play a significant role in improving patient outcomes. These approaches aim to address the emotional and psychological factors that may contribute to the development and exacerbation of both conditions. By providing patients with coping mechanisms and strategies to manage stress, healthcare professionals can help alleviate symptoms and improve overall quality of life.
In conclusion, the diagnosis and treatment of individuals with both vagus nerve disorders and SIBO require a comprehensive and multidisciplinary approach. Accurate diagnosis, achieved through specialized tests and a thorough evaluation of symptoms, is crucial for tailoring appropriate treatment strategies. By combining dietary modifications, prokinetic medications, and psychological interventions, healthcare professionals can effectively manage these conditions and improve patient outcomes.
The Importance of Holistic Health Approach
As our understanding of the link between vagus nerve disorders and SIBO evolves, it is crucial to recognize the significance of a holistic health approach in patient management. Adopting a holistic approach involves addressing not only the physical symptoms but also considering the impact of psychological, environmental, and lifestyle factors on the overall well-being of individuals affected by these interconnected conditions.
The Role of Diet and Lifestyle in Managing Vagus Nerve Disorders and SIBO
Encouraging individuals to make dietary and lifestyle modifications can have a profound impact on managing vagus nerve disorders and SIBO. Incorporating stress reduction techniques, regular exercise, and adequate sleep can help optimize vagus nerve function and minimize the risk of SIBO. Furthermore, a personalized diet that supports gastrointestinal health and reduces inflammation can minimize symptoms and aid in the prevention of bacterial overgrowth.
The Future of Neurogastroenterology: A Glimpse into the Future
With ongoing research and advancements in neurogastroenterology, our understanding of the link between vagus nerve disorders and SIBO continues to expand. Future developments may include targeted therapies that modulate the vagus nerve and restore optimal gut-brain communication, along with innovative diagnostic tools for more accurate and efficient detection of SIBO. By unraveling the complexities of this connection, healthcare professionals can enhance patient care and improve outcomes for those affected by vagus nerve disorders and SIBO.