The vagus nerve, also known as the tenth cranial nerve, plays a significant role in the regulation of various bodily functions, including digestion. This article aims to provide a comprehensive understanding of the vagus nerve and its intricate involvement in digestive disorders.
An Overview of the Vagus Nerve
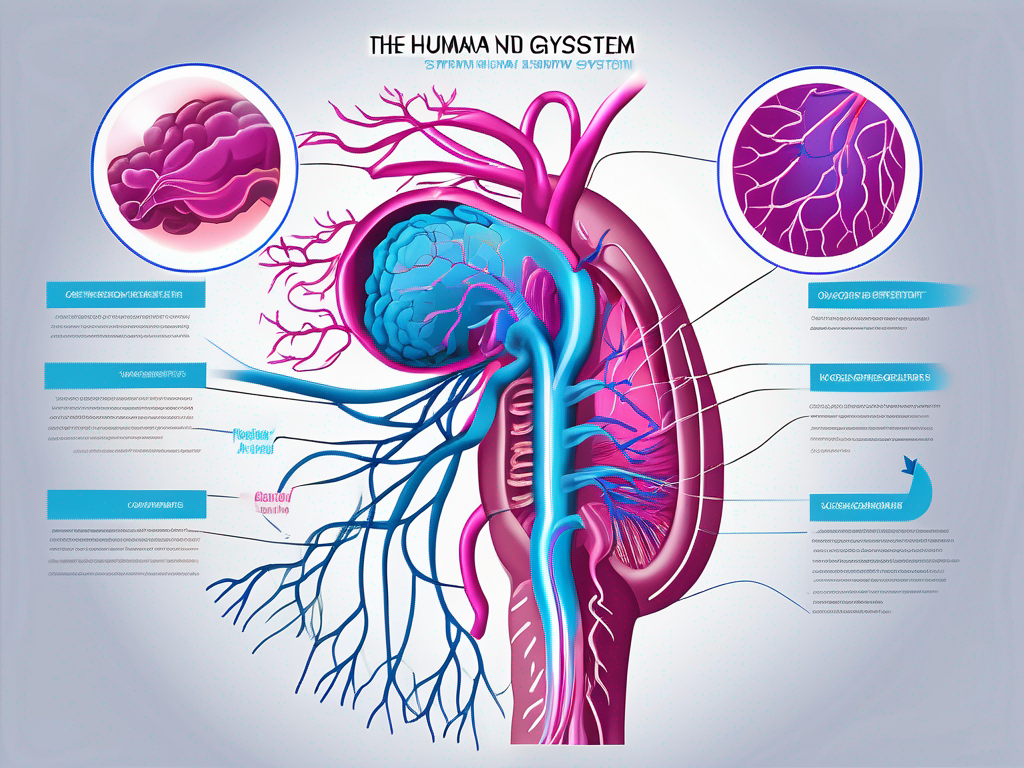
The vagus nerve is a long, wandering nerve that originates from the brainstem and extends down to the abdomen. It is responsible for transmitting signals between the brain and various organs and muscles throughout the body. As a key component of the parasympathetic nervous system, the vagus nerve controls involuntary bodily functions such as heart rate, breathing, and digestion.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It is named after the Latin word “vagus,” meaning “wandering,” due to its extensive distribution throughout the body. This nerve branches out into multiple smaller nerves, reaching organs such as the heart, lungs, stomach, liver, and intestines.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of both sensory and motor fibers. Sensory fibers transmit signals from organs, such as the stomach and intestines, to the brain, allowing us to perceive sensations like fullness or pain. Motor fibers, on the other hand, relay signals from the brain to the organs, regulating their functions.
One crucial function of the vagus nerve is to stimulate the release of digestive enzymes and gastric acid, essential for breaking down food into nutrients. It also controls the rhythmic contractions of the gastrointestinal muscles, facilitating the movement of food along the digestive tract.
In addition to its role in digestion, the vagus nerve plays a significant role in regulating heart rate. It helps to slow down the heart rate during periods of rest and relaxation, promoting a state of calmness. This is why deep breathing exercises and other relaxation techniques can activate the vagus nerve and induce a sense of tranquility.
The Vagus Nerve and the Autonomic Nervous System
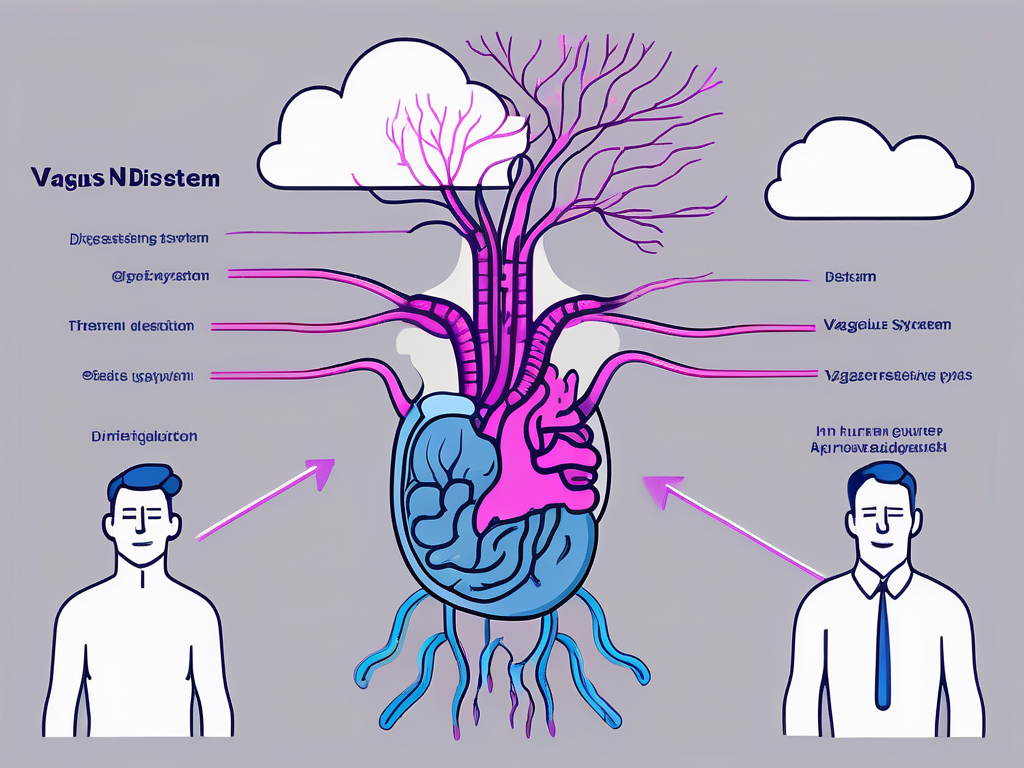
The vagus nerve is an integral part of the autonomic nervous system, which regulates bodily functions outside of voluntary control. It works in harmony with the sympathetic nervous system, its counterpart responsible for the body’s “fight or flight” response.
While the sympathetic nervous system increases heart rate and diverts blood flow away from the digestive system during times of stress, the vagus nerve has the opposite effect. It promotes rest and relaxation, enabling the body to focus on essential functions such as digestion and optimal nutrient absorption.
In addition to its role in digestion and heart rate regulation, the vagus nerve also influences other bodily functions. It helps to control respiratory functions, such as the rate and depth of breathing. It plays a role in regulating blood pressure, maintaining homeostasis within the body. Furthermore, the vagus nerve is involved in the release of certain hormones, such as oxytocin, which is responsible for promoting feelings of bonding and social connection.
Research has also shown that the vagus nerve plays a role in the body’s immune response. It helps to regulate inflammation and modulate the immune system’s activity, contributing to overall health and well-being.
Overall, the vagus nerve is a remarkable component of the nervous system, with its extensive reach and influence on various bodily functions. Understanding its anatomy and function can provide valuable insights into the intricate workings of the human body.
The Vagus Nerve’s Impact on Digestion
The vagus nerve plays a crucial role in coordinating the various stages of digestion, from the sight and smell of food to the final absorption of nutrients. Dysfunction of the vagus nerve can disrupt this intricate process, leading to various digestive disorders.
The Vagus Nerve and Stomach Function
The vagus nerve controls the production and release of stomach acid and digestive enzymes, ensuring proper digestion and nutrient absorption. It also regulates the peristaltic movements of the stomach, which churn and mix food with digestive juices.
When the vagus nerve is functioning optimally, it sends signals to the stomach to secrete an adequate amount of stomach acid and digestive enzymes. This allows for the breakdown of food into smaller, more manageable particles, facilitating the absorption of nutrients in the small intestine.
However, in cases of vagus nerve dysfunction, stomach acid production may be impaired. This can lead to insufficient breakdown of food and subsequent malabsorption. The undigested food particles can cause discomfort and bloating, while the lack of nutrient absorption can result in deficiencies and other health issues.
Furthermore, the vagus nerve’s control over the peristaltic movements of the stomach ensures that food is properly mixed with digestive juices. This process is crucial for breaking down food into a semi-liquid form called chyme, which can be easily transported to the small intestine for further digestion and absorption.
When the vagus nerve is not functioning properly, the peristaltic movements may become irregular or sluggish. This can lead to delayed gastric emptying, where food remains in the stomach for longer periods than necessary. The prolonged presence of food in the stomach can cause symptoms such as indigestion, bloating, and discomfort.
The Vagus Nerve and Intestinal Function
The vagus nerve extends its influence to the intestines, where it regulates the movement of digested food and absorption of nutrients. Dysfunction of the vagus nerve can disrupt this delicate balance, potentially leading to conditions such as constipation, diarrhea, and malabsorption disorders.
When the vagus nerve is functioning properly, it sends signals to the intestines to contract and relax in a coordinated manner, allowing for the smooth movement of digested food. This rhythmic motion, known as peristalsis, helps propel the food through the intestines, facilitating nutrient absorption.
In cases of vagus nerve dysfunction, the coordination of intestinal contractions may be disrupted. This can result in irregular or weakened peristalsis, leading to digestive issues such as constipation or diarrhea. Constipation occurs when the contractions are too weak, causing a delay in the passage of stool. On the other hand, diarrhea can occur when the contractions are too strong and rapid, leading to loose and watery stools.
Additionally, vagus nerve dysfunction can also contribute to malabsorption disorders. The impaired coordination of intestinal contractions can affect the proper mixing of digested food with digestive enzymes and bile, hindering the absorption of nutrients. This can lead to deficiencies in essential vitamins, minerals, and other vital nutrients.
In some cases, vagus nerve dysfunction can cause a condition known as gastroparesis. Gastroparesis is characterized by delayed gastric emptying, where the stomach takes longer than usual to empty its contents into the intestines. This can result in symptoms like nausea, vomiting, and a feeling of fullness even after consuming small amounts of food.
Overall, the vagus nerve’s impact on digestion is extensive and vital. Its proper functioning ensures the smooth coordination of various digestive processes, from the initial breakdown of food in the stomach to the absorption of nutrients in the intestines. Dysfunction of the vagus nerve can disrupt this intricate balance, leading to a range of digestive disorders and symptoms.
Common Digestive Disorders Linked to the Vagus Nerve
Several digestive disorders have been closely associated with vagus nerve dysfunction. Understanding these conditions can shed light on the significance of the vagus nerve in digestive health.
Gastroparesis and the Vagus Nerve
Gastroparesis is a condition characterized by delayed gastric emptying, often caused by vagus nerve dysfunction. The vagus nerve, also known as the “wandering nerve,” is responsible for controlling the movement and contraction of the stomach muscles. When the vagus nerve is not functioning properly, the stomach muscles may not contract as efficiently, leading to a delay in the emptying of food from the stomach into the small intestine.
There are various factors that can contribute to the development of gastroparesis, including diabetes, autoimmune diseases, or surgical damage to the vagus nerve. In diabetes, high blood sugar levels can damage the vagus nerve over time, leading to impaired stomach motility. Autoimmune diseases, such as lupus or scleroderma, can also affect the vagus nerve and disrupt its normal function. Additionally, surgical procedures that involve the manipulation or removal of the vagus nerve can result in gastroparesis.
Common symptoms of gastroparesis include bloating, nausea, vomiting, and early satiety. These symptoms can significantly impact a person’s quality of life, as they may experience discomfort and difficulty in digesting food properly. Treatment for gastroparesis typically involves dietary modifications, such as consuming smaller, more frequent meals, and avoiding foods that are difficult to digest. Medications that help improve stomach motility, such as prokinetic agents, may also be prescribed. In severe cases, surgical interventions, such as gastric electrical stimulation or pyloroplasty, may be considered to improve gastric emptying.
Gastroesophageal Reflux Disease (GERD) and the Vagus Nerve
The vagus nerve plays a vital role in the regulation of the lower esophageal sphincter (LES), a muscular valve that separates the esophagus from the stomach and prevents the backflow of stomach acid into the esophagus. Dysfunction of the vagus nerve can weaken the LES, leading to the development of gastroesophageal reflux disease (GERD).
GERD is a chronic condition characterized by the frequent and persistent backflow of stomach acid into the esophagus. This can cause symptoms such as heartburn, regurgitation, and difficulty swallowing. The vagus nerve controls the relaxation and contraction of the LES, ensuring that it opens to allow food to pass into the stomach and closes to prevent acid reflux. When the vagus nerve is not functioning properly, the LES may remain relaxed for longer periods, allowing stomach acid to flow back into the esophagus.
Treatment options for GERD range from lifestyle modifications to medication and, in severe cases, surgical interventions. Lifestyle modifications may include avoiding trigger foods, maintaining a healthy weight, elevating the head of the bed, and avoiding lying down after meals. Medications such as proton pump inhibitors (PPIs) or H2 blockers can help reduce the production of stomach acid and alleviate symptoms. In some cases, surgical procedures like fundoplication or LINX device placement may be recommended to strengthen the LES and prevent acid reflux.
In conclusion, the vagus nerve plays a crucial role in maintaining proper digestive function. Dysfunction of the vagus nerve can lead to various digestive disorders, including gastroparesis and GERD. Understanding the connection between these conditions and the vagus nerve can help healthcare professionals develop effective treatment strategies and improve the overall digestive health of individuals affected by these disorders.
Diagnosing Vagus Nerve Disorders
Identifying vagus nerve dysfunction requires a thorough evaluation of symptoms and appropriate medical tests. Understanding the typical signs and diagnostic procedures can aid in the accurate diagnosis of these disorders.
Symptoms Indicating Vagus Nerve Dysfunction
Common symptoms of vagus nerve dysfunction include indigestion, bloating, heartburn, constipation, diarrhea, nausea, vomiting, and difficulty swallowing. These symptoms may indicate an underlying issue with the vagus nerve’s regulation of the digestive system.
It is essential to consult with a healthcare professional when experiencing persistent or severe symptoms to receive appropriate evaluation and treatment.
Medical Tests for Vagus Nerve Disorders
Medical tests used to diagnose vagus nerve disorders may include gastroenterological evaluations, imaging studies, and specialized tests such as gastric emptying studies or esophageal manometry.
Gastroenterological evaluations may involve endoscopies, which allow for a visual examination of the digestive tract to assess any structural abnormalities or signs of inflammation. Imaging studies, such as ultrasound or magnetic resonance imaging (MRI), can provide an in-depth view of the digestive organs and evaluate the condition of the vagus nerve.
Treatment Options for Vagus Nerve-Related Digestive Disorders
Managing vagus nerve-related digestive disorders involves a multidisciplinary approach, incorporating various treatment options tailored to individual needs.
Medication and Therapy for Vagus Nerve Disorders
Many vagus nerve disorders can be managed with medications aimed at improving digestion, reducing acid reflux, or enhancing stomach motility. Additionally, therapies such as biofeedback, meditation, or relaxation exercises can help modulate vagal function and promote overall gut health.
Surgical Interventions for Vagus Nerve Disorders
In cases where conservative measures fail to provide relief, surgical interventions may be considered for certain vagus nerve disorders. Procedures such as vagotomy or gastric electrical stimulation can be performed to help restore normal functioning of the digestive system.
In conclusion,
Understanding the role of the vagus nerve in digestive disorders is crucial for healthcare professionals and patients alike. The vagus nerve’s intricate network and its influence on the digestive system highlight its importance in maintaining optimal digestive health. By addressing vagus nerve dysfunction through appropriate diagnosis and tailored treatment options, healthcare providers can help alleviate the symptoms and improve the quality of life for individuals with vagus nerve-related digestive disorders.