The human body is a complex and intricate system, with various components working together to maintain optimal health and well-being. One such component is the vagus nerve, a vital part of the autonomic nervous system. The vagus nerve is responsible for regulating numerous bodily functions, including heart rate, digestion, and respiration. Understanding the role and function of the vagus nerve is crucial in comprehending the various disorders that can affect it, especially in the thoracic spine region.
Anatomy of the Vagus Nerve
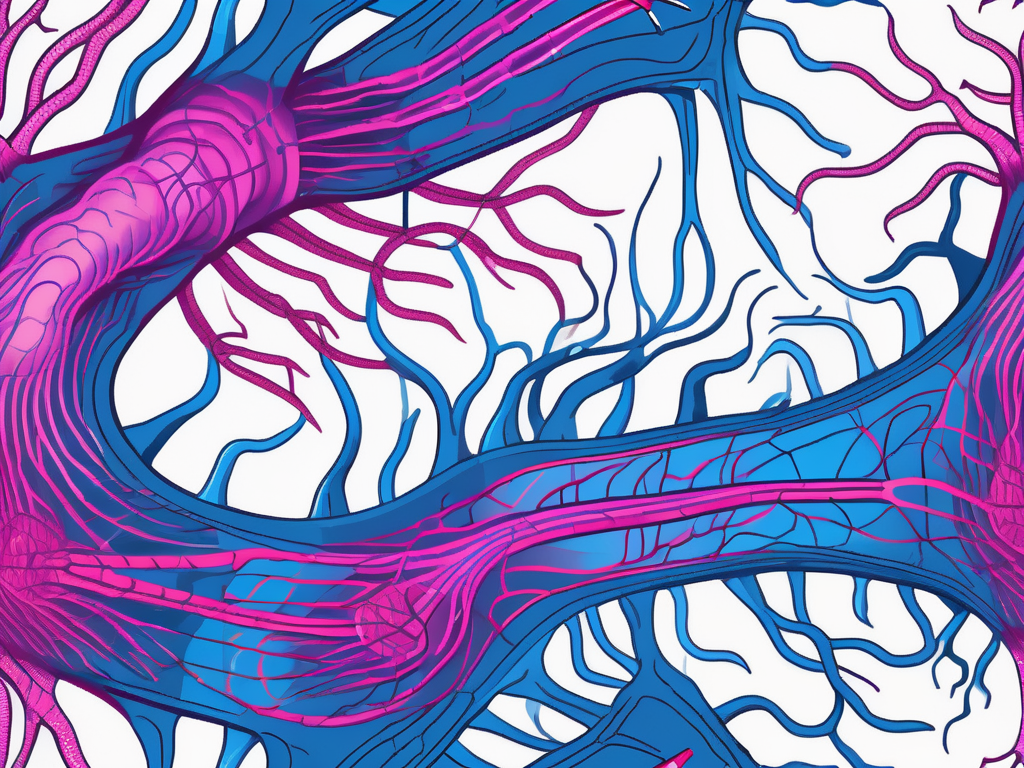
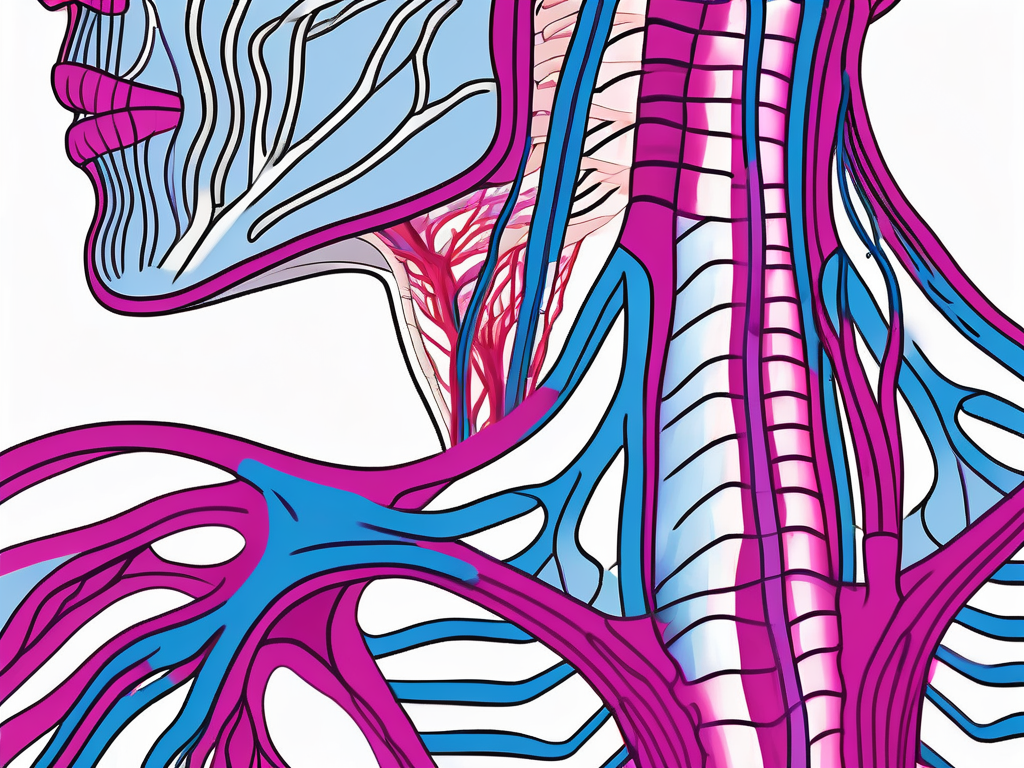
The vagus nerve, also known as the 10th cranial nerve, originates in the brainstem and extends down through the neck and thoracic spine to the abdomen. It is the longest cranial nerve in the body, branching out extensively to innervate various organs and structures. With both sensory and motor fibers, the vagus nerve plays a significant role in communication between the brain and the body.
The vagus nerve is a complex and fascinating structure that has captivated the attention of researchers and medical professionals for centuries. Its intricate network of fibers allows it to interact with numerous organs and systems in the body, making it a vital component of our overall health and well-being.
Role and Function of the Vagus Nerve
The vagus nerve primarily serves as the main parasympathetic nerve of the body, responsible for maintaining homeostasis and regulating vital functions. It acts as a bridge between the brain and various organs, transmitting signals that help control heart rate, digestion, breathing, and many other essential processes.
As a sensory nerve, the vagus nerve carries information from the organs back to the brain, providing feedback on their status and contributing to overall bodily awareness. For example, it relays information about the stretch and tension of the stomach, allowing the brain to regulate hunger and satiety. It also plays a crucial role in the gag reflex, alerting the brain to potential threats in the throat or airway.
Additionally, as a motor nerve, the vagus nerve controls the muscles involved in swallowing and speaking. It coordinates the intricate movements of the larynx, pharynx, and vocal cords, allowing us to produce speech and swallow food without difficulty. This intricate dance of muscle contractions and relaxations is orchestrated by the vagus nerve, ensuring smooth and efficient communication between the brain and the muscles involved.
Vagus Nerve Location in the Thoracic Spine
The vagus nerve courses through the thoracic spine region, situated close to the vertebral bodies and intervertebral discs. This location places it in proximity to various important structures, including the spinal cord, sympathetic ganglia, and blood vessels.
The close relationship between the vagus nerve and the spinal cord is particularly noteworthy. The spinal cord serves as a central hub for nerve signals traveling to and from the brain, and the vagus nerve is no exception. It sends and receives information through the spinal cord, allowing for efficient communication between the brain and the organs it innervates.
In addition to the spinal cord, the vagus nerve also interacts with sympathetic ganglia. These clusters of nerve cell bodies play a crucial role in the body’s fight-or-flight response, helping to mobilize resources and prepare for potential danger. The vagus nerve, with its parasympathetic function, acts as a counterbalance to the sympathetic nervous system, promoting relaxation and restorative processes.
Furthermore, the vagus nerve’s path through the thoracic spine brings it into close contact with blood vessels that supply oxygen and nutrients to the spinal cord and surrounding tissues. This close association highlights the importance of maintaining a healthy blood supply to support the proper functioning of the vagus nerve and the structures it innervates.
Any disruption or abnormalities in the thoracic spine region can potentially affect the function of the vagus nerve, leading to associated disorders. Conditions such as spinal cord injuries, herniated discs, or spinal stenosis can impinge on the nerve, causing symptoms such as difficulty swallowing, voice changes, or autonomic dysfunction.
In conclusion, the vagus nerve is a remarkable structure that plays a vital role in maintaining homeostasis and regulating various bodily functions. Its extensive network of fibers and its location in the thoracic spine highlight its complexity and importance in our overall well-being. Understanding the anatomy and function of the vagus nerve is crucial for healthcare professionals and researchers alike, as it paves the way for potential treatments and interventions to improve the health and quality of life for individuals with vagus nerve-related disorders.
Identifying Vagus Nerve Disorders
Identifying vagus nerve disorders can be challenging, as symptoms may vary depending on the specific condition and individual. However, recognizing common symptoms and utilizing diagnostic techniques can aid in the accurate diagnosis and management of these disorders.
Common Symptoms of Vagus Nerve Disorders
Individuals with vagus nerve disorders may experience a wide range of symptoms, which can affect different body systems. Common symptoms include difficulty swallowing, hoarseness, heart rhythm abnormalities, gastrointestinal disturbances, and respiratory issues. Moreover, some individuals may also exhibit symptoms of autonomic dysfunction, such as dizziness and fainting.
Difficulty swallowing, known as dysphagia, is a common symptom experienced by individuals with vagus nerve disorders. This can manifest as a feeling of food getting stuck in the throat or chest, making it challenging to eat or drink. Hoarseness, on the other hand, refers to a change in the voice quality, often characterized by a raspy or weak voice. It can occur due to the dysfunction of the vocal cords, which are innervated by the vagus nerve.
Heart rhythm abnormalities, also known as arrhythmias, are another common symptom of vagus nerve disorders. The vagus nerve plays a crucial role in regulating the heart rate and rhythm. When the vagus nerve is affected, it can lead to irregular heartbeats, palpitations, or even fainting spells. Gastrointestinal disturbances, such as nausea, vomiting, and abdominal pain, can also occur due to the vagus nerve’s involvement in the digestive system.
In addition to the symptoms mentioned above, respiratory issues can also be a manifestation of vagus nerve disorders. The vagus nerve helps control the muscles involved in breathing, and any dysfunction can lead to shortness of breath, difficulty breathing, or even respiratory failure in severe cases. Furthermore, individuals with vagus nerve disorders may experience symptoms of autonomic dysfunction, which can include dizziness, lightheadedness, and fainting episodes. These symptoms occur due to the disruption of the autonomic nervous system’s normal functioning, which is regulated in part by the vagus nerve.
Diagnostic Techniques for Vagus Nerve Disorders
Diagnosing vagus nerve disorders often involves a comprehensive evaluation of the patient’s medical history, physical examination, and specialized tests. These tests may include imaging studies, such as magnetic resonance imaging (MRI), to visualize the thoracic spine and identify any structural abnormalities or nerve impingement. Nerve conduction studies and electromyography can assess the electrical activity of the nerves and muscles, providing valuable information about their function.
During the medical history assessment, the healthcare provider will inquire about the patient’s symptoms, their duration, and any factors that worsen or alleviate them. They will also ask about the patient’s medical history, including any previous conditions or surgeries that may be relevant to the current symptoms. The physical examination may involve assessing the patient’s vital signs, performing neurological tests, and examining specific areas of concern, such as the throat or chest for swallowing difficulties or vocal cord abnormalities.
Imaging studies, such as MRI, can provide detailed images of the thoracic spine, which houses the vagus nerve. This can help identify any structural abnormalities, such as herniated discs or tumors, that may be compressing or irritating the nerve. Nerve conduction studies and electromyography involve the use of electrodes to measure the electrical activity of the nerves and muscles. These tests can help determine if there is any damage or dysfunction in the vagus nerve or its associated muscles.
Overall, a combination of medical history assessment, physical examination, and specialized tests is crucial in diagnosing vagus nerve disorders. By identifying the specific condition and understanding the individual’s symptoms, healthcare providers can develop an appropriate treatment plan to manage and alleviate the symptoms associated with vagus nerve disorders.
Types of Vagus Nerve Disorders
Vagus nerve disorders encompass a broad spectrum of conditions that can affect the normal functioning of the vagus nerve. The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating various bodily functions, including digestion, heart rate, and breathing. When the vagus nerve is disrupted, it can lead to a wide range of symptoms and complications.
Two notable types of vagus nerve disorders include vagus nerve damage and vagus nerve stimulation disorders.
Vagus Nerve Damage
Vagus nerve damage can occur due to various factors, such as trauma, infection, or compression. Traumatic injuries, such as car accidents or falls, can result in damage to the vagus nerve. Infections, such as Lyme disease or viral infections, can also affect the nerve’s function. Additionally, conditions like tumors or herniated discs can compress the vagus nerve, leading to impairments in its normal functioning.
When the vagus nerve is damaged, it can disrupt the proper transmission of signals along the nerve pathways. This disruption can result in impairments in the regulation of bodily functions. For example, individuals with vagus nerve damage may experience difficulties in digestion, leading to problems like gastroparesis, a condition where the stomach takes longer to empty its contents. They may also experience cardiovascular issues, such as abnormal heart rhythms or low blood pressure. Furthermore, respiratory problems, such as difficulty breathing or shortness of breath, can also arise due to vagus nerve damage.
Vagus Nerve Stimulation Disorders
Vagus nerve stimulation (VNS) is a therapeutic technique commonly used for treating certain neurological and psychiatric conditions. It involves the implantation of a device that delivers electrical impulses to the vagus nerve, helping to regulate abnormal brain activity. While VNS can be beneficial for many individuals, there are potential side effects associated with the procedure.
In some cases, individuals undergoing VNS treatment may develop stimulation-related side effects. These side effects can range from mild discomfort, such as hoarseness or coughing, to more severe complications. Voice changes, such as a change in pitch or quality, can occur due to the proximity of the vagus nerve to the vocal cords. Respiratory problems, such as shortness of breath or difficulty swallowing, can also arise as a result of vagus nerve stimulation.
It is important to note that the occurrence and severity of these side effects can vary among individuals. Some individuals may experience minimal side effects that are easily managed, while others may require adjustments to the stimulation settings or even removal of the device.
In conclusion, vagus nerve disorders encompass a wide range of conditions that can disrupt the normal functioning of the vagus nerve. Vagus nerve damage can occur due to trauma, infection, or compression, leading to impairments in the regulation of bodily functions. Vagus nerve stimulation disorders can arise as a result of therapeutic interventions, such as VNS treatment, and can cause side effects ranging from mild discomfort to more severe complications. Understanding these different types of vagus nerve disorders is essential for proper diagnosis, treatment, and management of these conditions.
Treatment Options for Vagus Nerve Disorders
Effective management of vagus nerve disorders typically involves a multifaceted approach, incorporating various treatment modalities tailored to the individual’s specific condition and needs.
Medication and Drug Therapies
Medication and drug therapies are commonly employed in the management of vagus nerve disorders, aiming to alleviate symptoms and improve overall function. Depending on the underlying cause of the disorder, different medications may be prescribed, such as pain relievers, anti-inflammatory drugs, or medications targeting specific conditions that affect the vagus nerve.
Surgical Interventions for Vagus Nerve Disorders
In cases where conservative measures are insufficient or the condition is severe, surgical interventions may be considered. Surgical procedures, such as vagus nerve decompression or neuromodulation, can help alleviate compression or stimulate the nerve, respectively. These procedures should be performed by experienced healthcare professionals in specialized centers, ensuring optimal outcomes and minimizing risks.
The Impact of Vagus Nerve Disorders on Quality of Life
Vagus nerve disorders can have a significant impact on an individual’s quality of life, affecting both physical and psychological well-being.
Physical Implications of Vagus Nerve Disorders
Physical implications of vagus nerve disorders can manifest as difficulties in daily activities, such as eating and speaking. Gastrointestinal disturbances, cardiovascular abnormalities, and respiratory issues can also limit an individual’s functionality and cause distressing symptoms. Proper management and supportive care are essential in addressing these physical implications and promoting overall well-being.
Psychological Effects of Vagus Nerve Disorders
Vagus nerve disorders can also contribute to psychological effects, including anxiety and depression. The disruption of normal bodily functions and the chronic nature of some vagus nerve disorders can impact an individual’s mental health and emotional well-being. Psychological support, counseling, and stress management techniques can play a vital role in enhancing the psychological resilience and coping abilities of individuals affected by these disorders.
In conclusion, understanding vagus nerve disorders in the thoracic spine is essential for proper recognition, diagnosis, and management of these conditions. The anatomy and function of the vagus nerve, common symptoms, diagnostic techniques, and treatment options all contribute to a comprehensive understanding of these disorders. Moreover, acknowledging the physical and psychological impact of vagus nerve disorders emphasizes the need for holistic care that integrates medical interventions and supportive therapies. By advancing our knowledge and awareness, we can strive towards improved outcomes and enhanced quality of life for individuals affected by vagus nerve disorders.