The vagus nerve, also known as the tenth cranial nerve or CN X, plays a crucial role in regulating various functions of the body. From controlling heart rate and digestion to influencing mood and immune response, the vagus nerve is an integral part of the autonomic nervous system. However, when this vital nerve becomes compromised, it can lead to a range of disorders that can significantly impact an individual’s quality of life. Understanding the underlying causes of vagus nerve disorders is essential for accurate diagnosis and effective treatment.
The Role of the Vagus Nerve in the Body
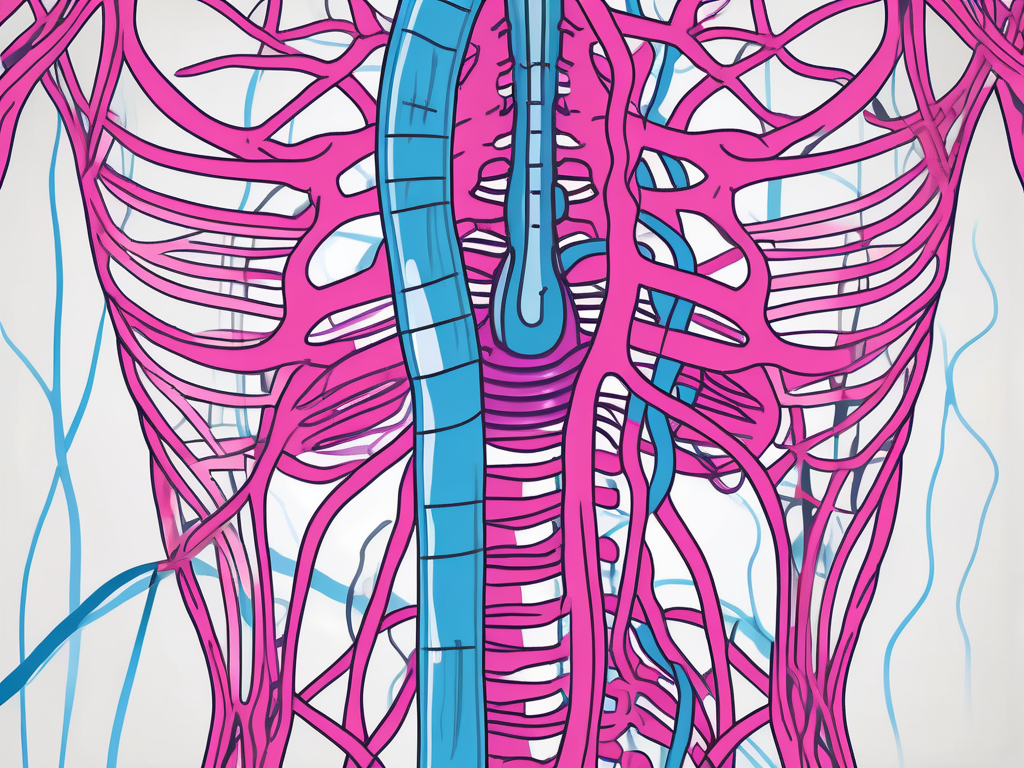
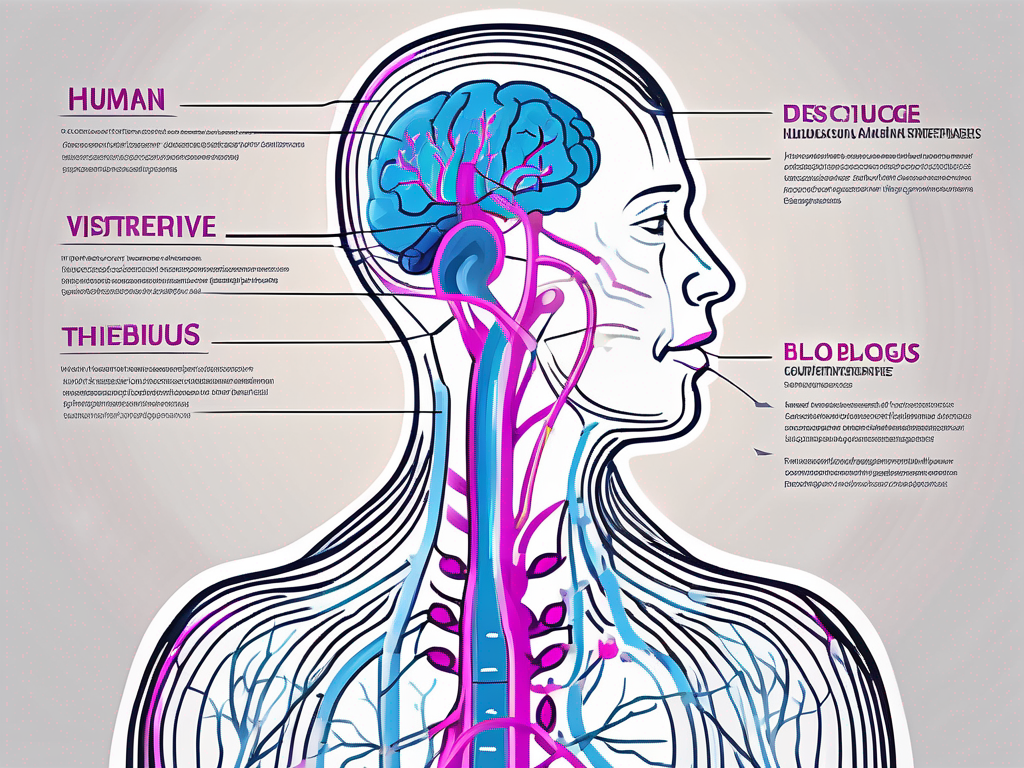
The vagus nerve is the longest cranial nerve in the body, extending from the brainstem down through the neck and chest to the abdomen. It is responsible for carrying sensory and motor information between the brain and various organs and tissues. As a major component of the parasympathetic division of the autonomic nervous system, the vagus nerve helps regulate involuntary bodily functions.
The vagus nerve plays a crucial role in maintaining the body’s overall balance and well-being. It acts as a communication highway, transmitting signals between the brain and different organs, allowing for coordinated and efficient functioning.
Anatomy and Functions of the Vagus Nerve
The vagus nerve consists of both afferent and efferent fibers, meaning it carries signals from the organs to the brain and vice versa. Afferent fibers transmit sensory information from organs such as the heart, lungs, and digestive system to the brain. These signals provide the brain with important feedback about the body’s internal environment, allowing it to make necessary adjustments to maintain optimal functioning.
For example, when the heart senses a decrease in oxygen levels, it sends signals through the vagus nerve to the brain. In response, the brain can initiate appropriate actions, such as increasing the heart rate or adjusting blood flow, to ensure adequate oxygen supply to the body’s tissues.
Efferent fibers, on the other hand, carry motor commands from the brain to the organs, controlling processes like digestion, heart rate, and breathing. The vagus nerve plays a crucial role in regulating these essential bodily functions, ensuring they occur in a coordinated and balanced manner.
The Vagus Nerve and the Autonomic Nervous System
The autonomic nervous system consists of the sympathetic and parasympathetic divisions, which work together to maintain homeostasis in the body. While the sympathetic division is responsible for the “fight or flight” response, the parasympathetic division, controlled predominantly by the vagus nerve, promotes relaxation and restoration.
When activated, the parasympathetic division through the vagus nerve helps counteract the effects of stress and promotes a state of calmness. It slows heart rate, enhances digestion, and promotes overall well-being. This is why activities such as deep breathing, meditation, and gentle exercise can activate the vagus nerve and induce a sense of relaxation and tranquility.
Furthermore, the vagus nerve also plays a role in regulating inflammation in the body. It has been shown to have anti-inflammatory effects, helping to reduce the body’s immune response and prevent excessive inflammation. This is particularly important in conditions such as autoimmune diseases, where the immune system mistakenly attacks healthy tissues.
In addition to its role in regulating bodily functions, the vagus nerve has also been linked to various mental health conditions. Studies have shown that vagus nerve stimulation can have positive effects on conditions such as depression and anxiety. By modulating the activity of the vagus nerve, it is possible to influence mood and emotional well-being.
In conclusion, the vagus nerve is a vital component of the body’s nervous system, responsible for carrying signals between the brain and various organs. Its role in regulating involuntary bodily functions and promoting overall well-being cannot be overstated. Understanding the intricate workings of the vagus nerve opens up new possibilities for therapeutic interventions and the promotion of optimal health.
Identifying Vagus Nerve Disorders
Vagus nerve disorders can manifest in various ways, often presenting with a combination of physical and psychological symptoms. It is important to be aware of these symptoms to facilitate early detection and appropriate management.
The vagus nerve, also known as the tenth cranial nerve, is the longest cranial nerve in the body. It originates in the brainstem and extends down to the abdomen, innervating various organs along the way. This nerve plays a crucial role in regulating many bodily functions, including heart rate, digestion, and mood.
Symptoms Associated with Vagus Nerve Disorders
Common symptoms of vagus nerve disorders include irregular heart rate, difficulty swallowing, gastrointestinal disturbances, such as bloating and constipation, excessive sweating, and dizziness or fainting spells. Additionally, individuals may experience mood changes, anxiety, depression, or difficulties with memory and concentration.
Irregular heart rate, also known as arrhythmia, can occur when the vagus nerve is not functioning properly. This can lead to palpitations, a racing heart, or a feeling of skipped beats. Difficulty swallowing, known as dysphagia, can be a result of vagus nerve dysfunction affecting the muscles responsible for swallowing. Gastrointestinal disturbances, such as bloating and constipation, can arise due to the vagus nerve’s role in regulating digestion.
Excessive sweating, medically known as hyperhidrosis, can be a symptom of vagus nerve disorders. The vagus nerve controls the sweat glands, and when it malfunctions, it can lead to abnormal sweating patterns. Dizziness or fainting spells, also known as syncope, can occur when the vagus nerve fails to regulate blood pressure effectively.
In addition to the physical symptoms, vagus nerve disorders can also impact an individual’s mental health. Mood changes, anxiety, and depression can arise due to the intricate connection between the vagus nerve and the brain. The vagus nerve carries signals between the brain and various organs, including those involved in mood regulation.
Common Vagus Nerve Disorders
While there are several vagus nerve disorders, two of the most prevalent conditions are vagus nerve neuropathy and vagus nerve irritation. Vagus nerve neuropathy refers to damage or dysfunction of the nerve, often resulting from trauma, infections, or autoimmune diseases. This condition can lead to a wide range of symptoms, depending on the location and severity of the nerve damage.
Vagus nerve irritation, on the other hand, can occur due to inflammation or compression of the nerve by neighboring structures. This can be caused by conditions such as gastroesophageal reflux disease (GERD), where stomach acid flows back into the esophagus and irritates the vagus nerve. Other potential causes of vagus nerve irritation include tumors, infections, or surgical procedures in the vicinity of the nerve.
It is important to note that diagnosing vagus nerve disorders can be challenging, as the symptoms can overlap with other medical conditions. A thorough medical evaluation, including a detailed medical history, physical examination, and possibly specialized tests, may be necessary to determine the underlying cause of the symptoms.
In conclusion, vagus nerve disorders can have a significant impact on an individual’s physical and mental well-being. Recognizing the symptoms associated with these disorders is crucial for early detection and appropriate management. If you suspect you may be experiencing vagus nerve dysfunction, it is important to consult with a healthcare professional for an accurate diagnosis and tailored treatment plan.
The Underlying Causes of Vagus Nerve Disorders
Vagus nerve disorders can have multifactorial causes, with genetic factors and environmental triggers playing significant roles in their development.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the autonomic nervous system. It is responsible for regulating various bodily functions, including heart rate, digestion, and respiratory rate. When the vagus nerve becomes disrupted or dysfunctional, it can lead to a wide range of symptoms and health issues.
Genetic Factors Influencing Vagus Nerve Disorders
Recent research suggests that variations in certain genes may predispose individuals to vagus nerve disorders. Gene mutations affecting the development or function of the vagus nerve can disrupt its normal signaling pathways, leading to dysfunction and the onset of various symptoms.
One particular gene of interest is the cholinergic receptor nicotinic alpha 7 subunit gene (CHRNA7). Studies have shown that variations in this gene can increase the risk of developing vagus nerve disorders. The CHRNA7 gene is involved in the production of a receptor protein that plays a crucial role in the transmission of signals along the vagus nerve. Any abnormalities in this gene can impair the functioning of the receptor, leading to vagus nerve dysfunction.
In addition to CHRNA7, other genes involved in the development and maintenance of the vagus nerve have also been implicated in vagus nerve disorders. These include genes responsible for the formation of the myelin sheath, a protective covering around nerve fibers. Mutations in these genes can disrupt the integrity of the myelin sheath, affecting the conduction of nerve impulses along the vagus nerve.
Environmental Triggers for Vagus Nerve Disorders
Environmental factors, such as infections, autoimmune diseases, and physical trauma, can also contribute to vagus nerve disorders. Infections like Lyme disease, HIV, and herpes zoster virus can directly affect the nerve, causing inflammation and damage. The inflammatory response triggered by these infections can disrupt the normal functioning of the vagus nerve, leading to symptoms such as pain, gastrointestinal disturbances, and heart rhythm abnormalities.
Autoimmune disorders involving the nervous system, such as Guillain-Barre syndrome, can also lead to vagus nerve dysfunction. In Guillain-Barre syndrome, the immune system mistakenly attacks the myelin sheath of peripheral nerves, including the vagus nerve. This immune-mediated damage can result in a range of symptoms, including muscle weakness, numbness, and difficulty breathing.
Physical trauma, such as a severe blow to the head or neck, can also impact the vagus nerve. The force of the trauma can disrupt the nerve fibers or compress the nerve, leading to dysfunction. In some cases, surgical procedures involving the neck or chest area may inadvertently damage the vagus nerve, causing complications post-surgery.
It is important to note that vagus nerve disorders can have complex and interconnected causes. Genetic predisposition may increase susceptibility to environmental triggers, while environmental factors can exacerbate underlying genetic vulnerabilities. Understanding the underlying causes of vagus nerve disorders is crucial for developing effective treatment strategies and improving patient outcomes.
Diagnostic Procedures for Vagus Nerve Disorders
Accurate diagnosis of vagus nerve disorders is crucial for developing effective treatment strategies. The diagnostic process typically involves a combination of clinical examination, medical history assessment, and various imaging and laboratory tests.
Clinical Examination and History
During the clinical examination, healthcare professionals will evaluate the patient’s symptoms and perform a thorough physical examination. This examination may include assessing the patient’s vital signs, such as heart rate and blood pressure, as well as conducting neurological tests to evaluate the function of the vagus nerve.
Healthcare providers will also inquire about the individual’s medical history, including past illnesses, medications, and any potential exposure to environmental triggers. This comprehensive assessment helps in identifying any underlying conditions or factors that may contribute to the development of vagus nerve disorders.
Imaging Tests
To further investigate and confirm vagus nerve disorders, healthcare providers may order imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to visualize the nerve and surrounding structures. These imaging techniques provide detailed images of the anatomy and can help identify any structural abnormalities or lesions that may be affecting the vagus nerve.
Magnetic resonance imaging (MRI) uses a powerful magnetic field and radio waves to create detailed images of the body. It can provide high-resolution images of the brain, neck, and chest, allowing healthcare professionals to assess the vagus nerve and its surrounding structures.
Computed tomography (CT) scans use X-rays and computer technology to generate cross-sectional images of the body. This imaging technique can provide detailed images of the bones, soft tissues, and blood vessels, aiding in the diagnosis of vagus nerve disorders.
Laboratory Tests
In addition to imaging tests, laboratory tests may be conducted to assess nerve function and identify any abnormalities. Blood tests can help evaluate the levels of certain substances in the blood that may indicate nerve damage or inflammation. These tests may include measuring inflammatory markers, such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), which can indicate the presence of an underlying inflammatory condition.
Nerve conduction studies are another type of laboratory test that can be performed to assess the function of the vagus nerve. During this test, small electrodes are placed on the skin overlying the nerve, and a small electrical impulse is applied. The response of the nerve is then recorded, allowing healthcare professionals to evaluate the conduction of electrical signals along the nerve and identify any abnormalities.
In some cases, additional specialized tests may be performed to further evaluate the function of the vagus nerve, such as autonomic function tests or esophageal manometry. These tests can provide valuable information about the nerve’s role in regulating various bodily functions, such as heart rate, blood pressure, and digestion.
Overall, the combination of clinical examination, medical history assessment, imaging tests, and laboratory tests allows healthcare professionals to make an accurate diagnosis of vagus nerve disorders. This comprehensive approach ensures that appropriate treatment strategies can be developed to manage and alleviate the symptoms associated with these conditions.
Treatment Options for Vagus Nerve Disorders
Once a vagus nerve disorder has been diagnosed, various treatment options can be explored, aiming to alleviate symptoms and improve overall patient well-being.
Medication and Surgical Interventions
Medications such as pain relievers, anti-inflammatory drugs, and anticonvulsants may be prescribed to manage pain, inflammation, and other specific symptoms associated with vagus nerve disorders. In severe cases, surgical interventions, such as nerve decompression or neurostimulation, may be considered to relieve pressure on the nerve or restore its normal functioning.
Lifestyle Changes and Alternative Therapies
Complementary and alternative therapies, including acupuncture, yoga, meditation, and dietary modifications, can be beneficial in managing vagus nerve disorders. These approaches focus on promoting relaxation, reducing stress, and supporting overall nerve health. Lifestyle modifications, such as regular exercise, adequate sleep, and stress management techniques, are also essential in managing symptoms and improving quality of life.
By understanding the underlying causes of vagus nerve disorders, healthcare professionals can better diagnose and treat these conditions effectively. Research into the genetic and environmental factors influencing vagus nerve disorders continues to advance, leading to improved treatment options and potential preventive measures in the future.