Vagus nerve disorders can be complex and require specialized medical care. Understanding the doctors who treat these conditions is essential to ensure proper diagnosis and management. In this article, we will explore the medical specialties involved in treating vagus nerve disorders, the diagnostic process, treatment options, and the importance of a multidisciplinary approach to these conditions.
Understanding Vagus Nerve Disorders
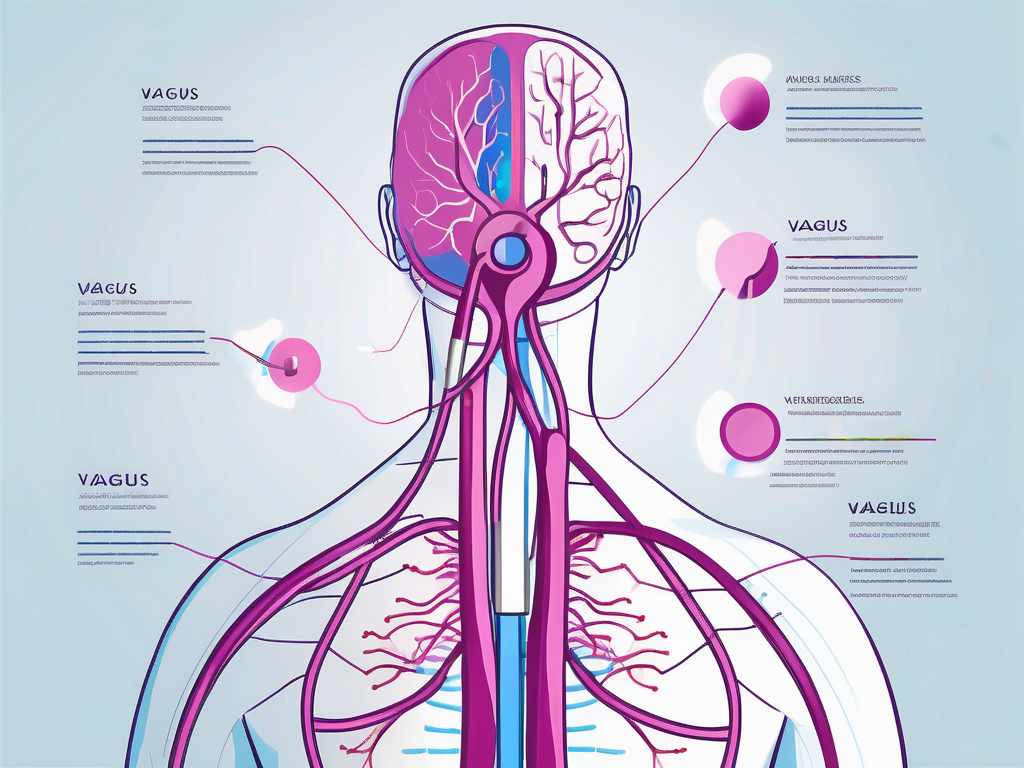
Vagus nerve disorders refer to conditions that affect the functioning of the vagus nerve, the longest cranial nerve in the body. The vagus nerve plays a vital role in regulating various bodily functions, including heart rate, digestion, and breathing. When this nerve is disrupted or damaged, it can lead to a wide range of symptoms and health issues.
The Role of the Vagus Nerve in the Body
The vagus nerve, also known as the “wandering nerve,” has branches that reach various organs and tissues in the body. It carries signals from the brain to these organs, influencing their functioning. The vagus nerve has both sensory and motor functions, allowing it to sense changes in the body and send signals to initiate appropriate responses.
For example, when you eat a meal, the vagus nerve helps stimulate the release of digestive enzymes and increases blood flow to the digestive organs, promoting efficient digestion. It also plays a crucial role in regulating heart rate by transmitting signals from the brain to the heart, helping to maintain a steady rhythm.
In addition to its role in digestion and heart rate regulation, the vagus nerve is involved in controlling breathing. It sends signals to the diaphragm and other respiratory muscles, allowing for smooth and coordinated breathing patterns. This nerve also plays a role in controlling inflammation in the body, as it can communicate with immune cells and regulate the release of anti-inflammatory substances.
Common Vagus Nerve Disorders
Several medical conditions can affect the vagus nerve, resulting in various disorders. Some common vagus nerve disorders include:
- Vagus nerve damage
- Vagus nerve compression
- Vagus nerve stimulation
Vagus nerve damage can occur due to trauma, surgery, or certain medical conditions such as diabetes or autoimmune diseases. This damage can disrupt the normal functioning of the nerve, leading to symptoms such as difficulty swallowing, hoarseness, or a weak cough. In severe cases, it can even cause paralysis of the vocal cords or affect the muscles involved in swallowing, leading to aspiration pneumonia.
Vagus nerve compression refers to the compression or entrapment of the nerve by surrounding structures, such as blood vessels or tumors. This compression can result in symptoms such as chronic pain, difficulty speaking or swallowing, and gastrointestinal issues like nausea, vomiting, or bloating. Treatment for vagus nerve compression may involve surgical intervention to relieve the pressure on the nerve.
Vagus nerve stimulation is a therapeutic approach used to treat certain neurological conditions, such as epilepsy or depression. It involves the implantation of a device that delivers electrical impulses to the vagus nerve, helping to regulate abnormal brain activity or improve mood. This treatment option has shown promising results in reducing seizure frequency and improving mood in individuals who have not responded well to other treatments.
Each of these conditions has its unique symptoms and requires specific treatment approaches. It is essential to consult with a healthcare professional for an accurate diagnosis and appropriate management of vagus nerve disorders.
The Medical Specialties Involved in Treating Vagus Nerve Disorders
The diagnosis and treatment of vagus nerve disorders often require collaboration among medical specialists from different fields. The following medical specialties play a crucial role in treating these conditions:
Neurologists and Vagus Nerve Disorders
Neurologists specialize in diagnosing and treating conditions related to the nervous system, including those affecting the vagus nerve. They utilize various diagnostic tests, such as nerve conduction studies and electromyography, to assess nerve function. Neurologists often work closely with other specialists to develop treatment plans tailored to each patient’s specific needs.
When a patient presents with symptoms such as difficulty swallowing, voice changes, or unexplained fainting, neurologists are trained to conduct a thorough examination to determine if the vagus nerve is involved. They may also order additional tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, to identify any underlying causes or structural abnormalities that may be impacting the nerve’s function.
Once a diagnosis is made, neurologists may prescribe medications to manage symptoms and improve nerve function. They may also recommend physical therapy or other non-invasive treatments to help patients regain control over their bodily functions.
The Role of ENT Specialists
Ear, nose, and throat (ENT) specialists, also known as otolaryngologists, are trained to diagnose and treat disorders that affect the head and neck area, including the vagus nerve. They can assess any underlying structural issues, such as tumors or infections, that may be affecting the nerve.
When a patient presents with symptoms such as hoarseness, difficulty swallowing, or recurrent throat infections, ENT specialists are often consulted to evaluate the function of the vagus nerve. They may perform a laryngoscopy, a procedure that allows them to visualize the throat and vocal cords, to identify any abnormalities or signs of nerve dysfunction.
In some cases, ENT specialists may recommend surgical interventions to relieve nerve compression or remove any abnormalities impacting its function. These procedures can range from minimally invasive techniques to more complex surgeries, depending on the severity and nature of the condition. ENT specialists work closely with neurologists and other healthcare professionals to ensure comprehensive and coordinated care for patients with vagus nerve disorders.
When to Consult a Cardiologist
In some cases, vagus nerve disorders may manifest as cardiovascular symptoms. When this occurs, it may be necessary to consult a cardiologist. Cardiologists specialize in diagnosing and treating conditions related to the heart.
When a patient presents with symptoms such as irregular heart rhythms, dizziness, or fainting spells, cardiologists can help determine if any cardiac issues are related to vagus nerve dysfunction. They may conduct tests such as electrocardiograms (ECGs) or echocardiograms to assess heart function and identify any abnormalities.
Based on the findings, cardiologists can recommend appropriate treatment options, which may include medications to regulate heart rhythms or surgical interventions to address any underlying cardiac conditions. They work closely with neurologists and other specialists to ensure a comprehensive approach to managing vagus nerve disorders that involve cardiovascular symptoms.
Collaboration among these medical specialties is essential in providing comprehensive care for patients with vagus nerve disorders. By working together, neurologists, ENT specialists, and cardiologists can leverage their expertise to accurately diagnose and effectively treat these complex conditions, ultimately improving the quality of life for patients.
The Diagnostic Process for Vagus Nerve Disorders
If you suspect you have a vagus nerve disorder, the diagnostic process typically involves multiple steps, including:
Initial Consultation and Symptoms
Your healthcare provider will start by collecting a detailed medical history and conducting a physical examination. This initial consultation is crucial in understanding your overall health and identifying any potential risk factors or underlying conditions that may contribute to vagus nerve disorders. During the consultation, be prepared to discuss your symptoms in detail, including their duration, intensity, and any triggers or patterns you have noticed. Your healthcare provider will carefully listen to your concerns and ask relevant questions to gain a comprehensive understanding of your condition.
Based on the information gathered during the consultation, further investigations may be recommended. These investigations aim to provide a more accurate diagnosis and determine the most appropriate course of treatment.
Diagnostic Tests and Procedures
To confirm a vagus nerve disorder, your healthcare provider may order specific tests, such as:
- Nerve conduction studies: This test measures the speed and strength of electrical signals traveling through your nerves. By assessing the conduction of the vagus nerve, healthcare providers can identify any abnormalities or disruptions in its function.
- Electromyography: This procedure involves the insertion of small, needle-like electrodes into the muscles controlled by the vagus nerve. By measuring the electrical activity of these muscles, healthcare providers can evaluate the nerve’s ability to stimulate muscle contractions and identify any potential issues.
- Magnetic resonance imaging (MRI): This imaging technique uses powerful magnets and radio waves to create detailed images of the structures within your body. An MRI can help visualize the vagus nerve and surrounding tissues, allowing healthcare providers to detect any structural abnormalities or sources of compression.
- Computed tomography (CT) scans: Similar to an MRI, CT scans provide detailed images of the body. These scans can be particularly useful in identifying any tumors, growths, or other structural abnormalities that may be affecting the vagus nerve.
- Endoscopy: This procedure involves the insertion of a thin, flexible tube with a camera and light source (endoscope) into your body. By guiding the endoscope through your digestive tract or respiratory system, healthcare providers can visually examine the vagus nerve and surrounding tissues, looking for any signs of inflammation, damage, or other abnormalities.
These tests help evaluate the structure and function of the vagus nerve and identify any underlying causes or abnormalities that may be contributing to your symptoms. It is important to note that the specific tests ordered may vary depending on your individual case and the suspected vagus nerve disorder.
Once the diagnostic process is complete and a diagnosis is confirmed, your healthcare provider will work with you to develop a personalized treatment plan tailored to your specific needs. Treatment options may include medication, lifestyle modifications, physical therapy, or, in some cases, surgical intervention.
Treatment Options for Vagus Nerve Disorders
Treating vagus nerve disorders involves a combination of interventions tailored to each individual’s specific needs and underlying condition. Vagus nerve disorders can manifest in various ways, such as gastroparesis, epilepsy, or even depression. Therefore, it is crucial to develop a comprehensive treatment plan that addresses the unique symptoms and challenges faced by each patient.
Medication and Drug Therapies
Medications are often prescribed to alleviate symptoms associated with vagus nerve disorders. These may include pain relievers, anti-inflammatory drugs, muscle relaxants, or medications to regulate heart rate or blood pressure. The choice of medication depends on the specific symptoms and underlying condition of the patient.
For individuals experiencing chronic pain due to vagus nerve disorders, pain relievers such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids may be prescribed. These medications work by reducing inflammation and blocking pain signals, providing much-needed relief.
In cases where the vagus nerve disorder affects the gastrointestinal system, medications like prokinetics may be prescribed. Prokinetics help stimulate the movement of food through the digestive tract, alleviating symptoms such as bloating, nausea, and vomiting.
For individuals with vagus nerve disorders that impact heart rate or blood pressure, medications such as beta-blockers or calcium channel blockers may be prescribed. These medications help regulate the cardiovascular system, ensuring optimal functioning.
Surgical Interventions
In cases where structural abnormalities or nerve compression are causing the disorder, surgical intervention may be necessary. Surgery aims to relieve pressure on the nerve or repair any damage. ENT specialists and neurosurgeons are typically involved in performing these procedures.
One common surgical procedure for vagus nerve disorders is vagus nerve stimulation (VNS). VNS involves implanting a device that delivers electrical impulses to the vagus nerve, helping regulate its activity. This procedure has shown promising results in managing conditions such as epilepsy and treatment-resistant depression.
In cases where nerve compression is the underlying cause of the disorder, surgical decompression may be performed. This involves relieving pressure on the affected nerve by removing any surrounding structures or tissues that may be compressing it.
Lifestyle Changes and Home Remedies
Alongside medical treatments, lifestyle changes and home remedies can help manage vagus nerve disorders. These measures aim to support overall well-being and improve the functioning of the vagus nerve.
Stress reduction techniques, such as meditation, deep breathing exercises, and yoga, can help calm the nervous system and reduce the impact of stress on the vagus nerve. These practices promote relaxation and can alleviate symptoms associated with vagus nerve disorders.
Regular exercise is also beneficial for individuals with vagus nerve disorders. Physical activity helps improve blood circulation, release endorphins, and reduce inflammation, all of which can positively impact the functioning of the vagus nerve.
A healthy diet plays a crucial role in supporting the overall health of individuals with vagus nerve disorders. Consuming a balanced diet that includes plenty of fruits, vegetables, whole grains, and lean proteins provides essential nutrients that support nerve health and overall well-being.
Adequate sleep is vital for the proper functioning of the nervous system, including the vagus nerve. Establishing a regular sleep routine and creating a sleep-friendly environment can help individuals with vagus nerve disorders get the rest they need to support their recovery.
It is important to note that while lifestyle changes and home remedies can be beneficial, they should not replace medical treatments. It is essential to consult with a healthcare provider who can provide personalized recommendations based on your specific condition.
The Importance of a Multidisciplinary Approach
Given the complexity of vagus nerve disorders, a multidisciplinary approach to treatment is often necessary. Collaborative care among different specialists ensures that all aspects of the condition are addressed comprehensively, leading to optimal outcomes for the patient.
Collaborative Care for Optimal Outcomes
Neurologists, ENT specialists, cardiologists, and other healthcare professionals work together to develop a treatment plan that takes into account each patient’s unique circumstances. This multidisciplinary approach allows for a holistic evaluation and comprehensive management of vagus nerve disorders.
The Role of the Patient in Treatment Plan
Active patient participation is essential in the treatment of vagus nerve disorders. By closely following the recommended treatment plan, adhering to lifestyle modifications, and maintaining regular communication with healthcare providers, patients can contribute significantly to their own recovery and overall well-being.
In conclusion, vagus nerve disorders require specialized medical care, and various medical specialists contribute to their diagnosis and treatment. Neurologists, ENT specialists, and cardiologists play key roles in managing these conditions. The diagnostic process involves a thorough evaluation, including physical examinations and specific tests. Treatment options may include medications, surgical interventions, and lifestyle modifications. A multidisciplinary approach involving collaboration among healthcare professionals is vital for optimal outcomes. By actively participating in their treatment plans, patients can improve their chances of recovery and enhance their overall quality of life.